In the endless hallway of the NICU, nurses shuffled from door to door. Yellow-toned ceiling lights flickered. My grandmother kept her eyes glued to the tiled floor.
I rested my arms on the ledge of the fogged window, swiping at it so I could make out every detail of what was inside.
My mother was much skinnier than when I’d last seen her, over six months previously. Her favorite band shirt used to sit snug against her skin. Now, she was drowning in it. Her belly showed no hint of having carried life. It was hard to believe the newborn nestled in her arms had just come out of her frail body.
My sister’s fingers wiggled toward our mother, almost mimicking the slow rhythm of the beeping monitors that watched over them. IV drips poked into her arms, tubes pushed oxygen into her nose, and patches pressed into her chubbed skin. She blew bubbles and looked right up at our mother. Their eyes met in a silent union, passing something somber back and forth—perhaps a goodbye.
That was in the spring of 2018. I was 14. I never saw them together again.
***
My father’s two-bed apartment was cramped. His pregnant sister, her boyfriend, and their toddler were staying with our family after losing their home. We lived off my father’s welfare check, barely making rent. Food stamps never seemed to cover enough to feed us all. We couldn’t afford heat. Most of the time, I’d stay with friends so I could get fed, shower and clean my clothes.
When I was home, I’d often find my father in his recliner, lost in his high, the floor littered with wrappers, cigarette butts and empty pill bottles, and the fridge empty aside from dried condiment crusts and molds.
I was doing what I could to get by, and I knew my father was too. He tried to find work, but nowhere would take someone on methadone. He loved me and took care of me in the ways he could.
She was silent for days, until I caught her whispering to my father, “I’m pregnant.”
My mother walked out in early 2017. This wasn’t unusual; it had happened on and off since I was a toddler. When she was around, it never felt that she was. I’d pester her for attention, to try to win her love. But even winning a smile or hug was hard. Her distance hurt, but I understood. I’d seen her emotionally torn apart and physically abused by every man she’d thought would be the one to finally save her.
Her return in December that year, from another man who’d hurt her I presumed, was different. She was skin and bones, with bruises up her body. Her eyes were dim. She was silent for days—until I caught her whispering to my father, as I watched from between the rails at the top of the staircase, “I’m pregnant.”
That was my tipping point. I couldn’t bear the thought of another child living through all of this—in fact, I couldn’t bear to live through it anymore, either. That night, I called some relatives and begged them to let me stay. Days later I left, cutting off communication with my parents.
I ended up living with those relatives for years. Perhaps they took me in out of the goodness of their hearts, but they sought to convince me to resent my parents, for getting high instead of taking care of me. They surveilled and controlled my every move, to turn me away from becoming like my “welfare-leeching, druggie parents.”
I still don’t know why they let me see my mother and newborn sister in the hospital. Perhaps they knew, like my grandmother who insisted I come, that this might be my only chance to meet my sister.
When I got back, I brought them piles of questions. They made clear to me that my mother’s feeble state, my sister’s long stay in the hospital and their impending separation were the result of my mother “relapsing”—that she cared more about “scoring drugs” than protecting her unborn child.
And this is what I assumed to be the truth, until a few months ago.
***
Five years after my youngest sister was born—five years of confusion, anger and fear after 14-year-old me watched their final tender moment together—I finally grew the courage to ask my mother what happened.
Getting to this point wasn’t easy for either of us.
After arriving at Stanford, having wealth and privilege shoved in my face, I felt worse than ever about what I’d been through. I longed for answers and for resolution with my parents, particularly my mother. I started calling, making slow efforts to have her be a part of my life. And after a while, it became routine for us to talk over the phone, often about the past.
“The clinic made me go through withdrawal throughout my entire pregnancy.”
One day, I asked her about the pregnancy, recalling how our relatives thought she was using.
“It never had anything to do with me using drugs,” my mother told me. “I was sick, which made the baby sick. And that’s because the clinic made me go through withdrawal throughout my entire pregnancy.”
By the time she was pregnant with my sister, she had been at the same methadone clinic for around 15 years. She’d been one of the first patients to walk through the doors the day it opened.
In her eyes, and to clinic staff, she’d been the perfect patient. She made it to all her counseling sessions. She had clean urines. She was friendly with the dosing nurses and the clinic director, and built a strong relationship with her counselor. She’d had her take-homes for years and never had a problem keeping them.
When her random monthly drug screening came back indicating that she was pregnant, her counselor was very sweet about it and congratulated her. But the counselor said nothing about what the methadone stabilization process would look like during the pregnancy.
At the time, she was at 49 milligrams, much lower than the dose she’d long been on. About five years earlier, an ex-boyfriend made her try to get off; she was at 3 mg by the end of their relationship. Getting back up to a dose that made her feel well took years; the clinic only allowed patients to go up a maximum of 5 mg at a time—if their request was approved by the doctor.
At 49 mg, she was still on a low dose compared to what most other people she knew at the clinic were receiving.
“If you go up, you know what’s gonna happen. You’re gonna have to come every day again.”
Considering all this, when my mother came back to her counselor a few weeks after learning she was pregnant, expressing her need for a higher dose because she was starting to experience symptoms of withdrawal, she expected they would raise her dose right away.
Her counselor wouldn’t allow her to go up by even 1 milligram.
“Right away,” my mother recalled, “my counselor’s like, ‘Well, if you go up, you know what’s gonna happen.’”
“And I’m like, ‘What do you mean?’”
“And she tells me, ‘Well, you’re gonna have to come every day again.’”
The threat shocked my mother. She began to explain that she couldn’t get to the clinic every day. It was two hours away from where she lived, and she had neither a car nor the income to afford other transportation. Just getting there every Monday to pick up her weekly take-homes was extremely burdensome.
But the counselor knew all of this already.
“My counselor told me that if I wanted to go up, I’d lose my take-homes because I’d be considered ‘unstable,’” my mother said. “But I was pregnant, and I knew I was going to get super-sick. They shouldn’t have been worried about me being ‘unstable’; they should have been worried about my baby inside me being unstable.”
She’d been through withdrawal plenty of times, and that wasn’t her main concern. It was about the baby, and the fact that she was going to go through withdrawal too. “How is it fair,” she asked me, “that the baby inside me has to suffer because the clinic wouldn’t let me up my dose?”
As the pregnancy progressed, she began losing a lot of weight. Her belly shrank. She was severely dehydrated and vomiting nonstop. Severe anxiety prevented her from being able to sleep.
“It got to the point where the baby inside me was kicking as if she was in pain and trying to get out,” she said. “The kicks were violent. It was terrifying. I was so sick that when I’d go to my baby-doctor appointments they’d send me to the ER, where I’d be hooked up to an IV all day—or for even two days. The clinic knew that I was being put in the ER for that, and they still didn’t care. It didn’t register that they were causing this harm.”
She kept going back to the clinic, asking for a higher dose, but they always denied her requests. Eventually she stopped asking, afraid they’d see this as “drug-seeking behavior” and take away her existing take-homes.
“It’s like they were making me go through withdrawal to pressure me into coming in every day, so they could make more money off me.”
Her pregnancy with me, while attending the same clinic, had been nothing like this. Before, she’d been able to go up in her dosage as much as she needed. And clinic staff had been extra cautious, she said, to make sure she wasn’t experiencing any withdrawal symptoms.
Back then, my mother and father had a car and an apartment together. She’d been working evenings cutting hair, and he was in school. Somehow they managed to make the two-hour drive to the clinic every morning.
They were determined to do everything they could to set up a good life for me. But the exhaustion cultivated by the clinic set in, and it all slowly began to fall apart. Their car: gone. Her job: gone. His college degree: gone. Their hopes and dreams for the future: gone.
Years later, the weekly take-homes they’d “earned” could not undo this.
“This pregnancy was so unique because of my take-home status,” my mother explained. “When I was going every day, they didn’t care how high they’d dose me. They treated me like gold when they could charge Medicaid every time I dosed in front of them. It’s like I had more freedom when I didn’t have take-homes.”
Being able to make that comparison informed her understanding of why things were different this time around. “I started to realize it wasn’t about them caring that being on too much methadone would hurt me or my baby,” she said. “It’s like they were making me go through withdrawal to pressure me into coming in every day, so they could make more money off me.”
I approached Dr. Bruce Trigg, an experienced clinician and former medical director of a methadone clinic in Tucson, Arizona, with my mother’s story, asking him how methadone providers should handle pregnancies.
He was shocked at how low a dose she’d been on at the start of her pregnancy.
Dr. Trigg made clear that dose increases during pregnancy are the medical standard.
“Forty-nine milligrams of methadone is nothing,” he said. “The therapeutic dose is 80-120 mg … So why would someone be stuck at 49 mg for a long time like that? It makes no sense—that’s only half the therapeutic dose.”
Trigg also made clear that dose increases during pregnancy are the medical standard. “Throughout pregnancy, especially in the third trimester, the body’s fluid volume increases, and there is no question that women need higher doses.”
During pregnancy, the person “should not be experiencing withdrawal, because if they’re in withdrawal, the fetus is in withdrawal,” he said. “And that’s exactly what you want to avoid and that’s exactly why you want them to be on an adequate dose.”
There is no rule for methadone clinics, Trigg said, that stipulates you must dose daily at the clinic in order to get your dose increased during pregnancy. What was really happening, he believes, was stigma.
“The assumption [among clinic staff] is often that the patient is trying to ‘get something out of us’—trying to get high or trying to get more methadone than they need,” he said. “But anyone with experience, who’s picked up any book about methadone and pregnancy, [should know that pregnant people] need more methadone.”
Taking patients’ requests seriously and communicating with other providers throughout a pregnancy are critical to ensuring best outcomes, he added.
“Ideally, your mom would have had an OB-GYN, who had some experience working with women [on methadone], and would have been in communication with the doctor at the methadone clinic,” he said. “But, the reality is, that is super-rare [because] methadone is a complete standalone system.”
***
Eight months into her pregnancy, my mother had her yearly exam at the clinic, and that’s where she met the new doctor. He was unable to tell that she was pregnant, and she had to explain the whole situation again. But when she did, he increased her dose without hesitation—raising it from 49 to 59 milligrams during the last month of her pregnancy at 5 mg intervals, as confirmed by the dose history provided by my mother’s current clinic counselor.
“And that’s all it took,” she told me. “So if their line the whole time was that I couldn’t go up without losing my take-homes because ‘It’s the rules,’ then how was that newer doctor at the end able to up me by 10 milligrams without taking my take-homes from me? They flat-out lied to me, and nobody took responsibility. The damage was done.”
Despite this increase, she still experienced symptoms of withdrawal. And just before she was due to give birth, a sonogram revealed she had only a quarter of the amniotic fluid that would normally be present. Because of this, she underwent an emergency C-section.
My sister was immediately put in the NICU, on constant watch for 20 days until her condition stabilized. My mother came to the hospital everyday to bathe her, change her diapers, feed her and spend as much time with her as she could.
She told me how hard it was to see her baby have to deal with these health problems. She cried out to me over the phone how badly she’d wished for a better life for my sisters and me, how she’d give her life for us.
I did everything I could to not break down in that moment, knowing how much she already gave up for us when she never should have had to.
“My body was so beaten down because of the withdrawal,” she told me. “I had no job, because I’d lose my insurance and wouldn’t be able to afford to stay at the clinic if I did [get one]. And even if I did, how was I supposed to bring a newborn baby to the clinic by myself?”
“So I decided to give her up for adoption,” she whispered, “so she could have a normal family that could actually take care of her. It hurt me to have to do that, but her wellbeing was more important than anything to me.”
Until recently, my mother heard nothing of her daughter. Then, a little over two years ago, she received a call.
At the last minute, a family friend had offered to take her baby in, so that my mother would still be able to see her. My mother went to court to sign over custody, thinking she could stay connected to her child. This didn’t end up being the case. And up until recently, my mother heard nothing of her daughter.
Then, a little over two years ago, she received a call from child services. Over the phone, the person assigned to the case told my mother that her daughter had been taken into custody by the state, after they’d deemed her previous living situation unfit. Then, without informing my mother, they had placed my sister with another family.
After that phone call, she felt helpless. Fighting for custody, to her, seems like a battle she could never win. The harm done by the clinic cannot be undone.
“I was furious that I wasn’t the first person they’d call in making the decision,” she said. “They’d called my ex-boyfriends, who weren’t even related to the baby, and asked them if they’d be willing to take her in before they even tried calling me.”
“I’d expressed that I wasn’t comfortable with the placement they’d decided on because I wanted her to be in a drug-free environment,” she said of that phone call. “And he made a sarcastic comment, asking me if I was trying to say that I was sober too. He knew from the case file that I was on methadone. So, it felt like he was saying that I was unfit to take care of her either, because I was on methadone.”
“It’s really hard on me thinking back and knowing that if it would have been different, my baby’s life, my life and your life could have been so much better,” she said.
One person’s decision to stabilize my mother on methadone properly during her pregnancy with me might have been what allowed me to arrive with no complications, to stay with my parents and away from foster care, and to have the honor of knowing my mother, her story, her bravery and her love.
But one person’s decision to not up her dose, to force my mother through withdrawal while she was pregnant, afforded my sister a much different reality, with consequences unforeseeable.
My mother lost her child. My sister lost her mother. And I lost my sister.
“I really hope I live to see the day that this system ends.”
“I’m trapped at the clinic like I’m a prisoner, and I have to just sit here and watch silently as the people that run this whole system do everything they can to make my life miserable, to line their own pockets with cash because they know I need my medicine,” my mother said.
“Imagine I didn’t have to be there every day and could just get my medicine at a pharmacy like everyone else; that I didn’t have to have a nurse watch me take my medicine because I’m seen as being untrustable; that I didn’t have to be watched while I peed in a cup every month to prove my worth to live with ‘clean’ piss.”
“Imagine I didn’t have to go through withdrawal for nine months and be told by everyone that I was a bad mother because of it—when all along it has always been the clinic’s fault.”
The thing is, she didn’t have to tell me to imagine it. I imagine it all the time. I imagine my mother sitting in the same position with my newborn sister—but instead of monitors, IVs, oxygen tubes and patches, they’re surrounded by bright pink balloons, bouquets of flowers and a pile of stuffed animals.
I imagine myself in that room. I imagine my mother telling me, “Isn’t she so beautiful?” I imagine her putting her in my arms, looking up at me and then down at her, cupping her cheek, and whispering, “Look, that’s your big sister. She’ll always be by your side—just like me.”
This could have been our reality, and maybe it still can be for someone else.
“I know so many parents who have suffered and continue to suffer because of how awful the clinic is to them,” my mother said. “It can’t stay this way. I hope I don’t spend the rest of my life stuck at the clinic. I really hope I live to see the day that this system ends—where methadone clinics are a thing of the past.”
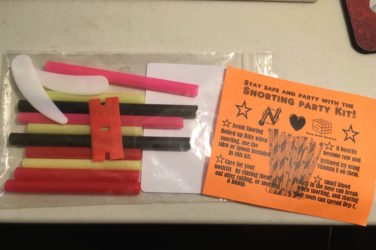
Photograph of the author’s mother with another sister, courtesy of the author




Show Comments