When someone dies without a doctor present, and they hadn’t seen a doctor anytime recently, a local medical examiner will be the one who decides how they died. “Unattended deaths” include all overdoses, and these days more and more unattended death reports include meth.
Post-mortem toxicology data show meth-involved death rates climbing sharply since around 2019, especially among people who died without housing. Which makes sense—there’s a ton of meth right now; more people are using it; more people have meth in their system at the moment they die.
Every state does death investigations differently, so every state’s death records are their own kind of mess. No one at the state or national level is in charge of aggregating this data, so it seems awfully dicey to project too much meaning onto what it says about the drug supply or the way people use it. But media outlets and police departments and harm reduction entities keep doing it anyway.
Full autopsies, where the body gets opened up, require a huge amount of time and labor. External autopsies do not.
Sixteen states and the District of Columbia have a centralized state-wide death records system; the rest do it by county. Some counties work in conjunction with their state medical examiner’s office. Some leave their death records entirely to the county coroners to figure out using independent examiners. Coroners don’t have to have any medical training; the positions are elected.
Full autopsies, where the body gets opened up, require a huge amount of time and labor. External autopsies do not—basically, someone looks at the body and writes down what they see, and then takes some vitreous and other fluids for toxicology analysis.
“We used to do full autopsies on all overdose deaths,” a toxicologist who signs off on drug death reports told Filter. They requested anonymity because the state medical examiner’s office they work for doesn’t allow them to speak to media. “But the system was getting so overwhelmed that we started doing urine immunoassays to see if they’re positive for [common substances like] meth, fentanyl or cocaine. If they are, it’s assumed it’s a drug overdose death and they usually don’t get cut open.”
If cause of death is undetermined, they have to get a full autopsy. If it’s attributed to drug toxicity, then they’re done.
Over the past decade, as state and federal governments escalated the drug war, laboratory expenses for controlled substance and toxicology analyses ballooned. Death reports backed up. Turnaround times for death certificates more than doubled.
Forensic pathologists—the physicians who specialize in death investigations and toxicology—burn out rapidly. Their caseloads are unsustainable enough that medical examiners’ offices get threatened with loss of accreditation for violating workplace standards. Today, the national pathologist shortage is so dire there are only around 500 of them handling unattended deaths for the whole country.
A pathologist will ultimately sign off on the report, but the person doing the actual investigating didn’t necessarily go to medical school. Medical examiners might be physician’s assistants, or EMTs. They get paid per body, and often cover multiple counties at a time.
As backlogs grow, so does the pressure to find a cause of death quickly. Without one, the medical examiner’s office can’t issue the death certificate, and without the death certificate the deceased’s next of kin can’t file life insurance claims. Prosecutors also need reliable death certificates to bring homicide charges to court, which is why in many states, like Oregon, law enforcement is deciding who gets a full autopsy and who was less important.
Because the purpose of a death investigation is to put something on the death certificate, medical examiners aren’t actually looking for the physical mechanism that made someone die; they’re looking for “the event or condition that precipitated it.”
Being sure about a cause of death allows the data to get sorted it into one of a handful of categories, like homicide, suicide or accidental. If a roving county medical examiner leaves a case undetermined, it has to get kicked up to a pathologist for a full autopsy. If they decide it was, for instance, acute drug toxicity—accidental death—then they’re done.
“The way that deaths are attributed is very hand-wavy,” the toxicologist said. “If there’s not another physical reason for them to be dead, and there was meth in their system, and we’ve got 42 of them we have to get through today, it becomes almost like a quick, lazy: meth death, meth death.”
The quality of someone’s death investigation is supposed to be the same whether they died in an apartment or a tent or a prison. But in reality, most of the factors that impact an autopsy are shaped by income and housing. How complete are the person’s medical records; did they have medical records at all; was their body exposed to the elements before it was found; did they die in a rural jurisdiction that does very few full autopsies; can their family afford a private one.
Some causes of death associated with meth use, like heart attack or stroke, are also associated with a bunch of other things, like blood clots, that you can’t see unless you open up the body to look. Others leave no physical evidence at all.
Death, like any other biological process we don’t fully understand, is often diagnosed by process of elimination. If the examiner doesn’t see an obvious cause, they go with one that seems reasonable to infer from the available evidence, which these days is often just a toxicology screen and a long look at the person who died. Cardiac arrhythmia or heat stroke don’t pop positive on a standard drug panel, but meth does.
It’s like, ‘Here’s someone that was found in a tent. We can’t contact their next of kin. They’ve got meth in their system; keep it moving. We’re not going to do an autopsy.'”
Death investigation errors happen all the time. But we still point to the meth toxicity data as if meth is the thing that’s going to get represented proportionally in all this, and then we circulate the headlines about deadly meth overdoses—with and without fentanyl—as if they say anything about what’s happening.
“If they had a heart death, I think [any meth] is going to get attributed as a cause of death. Because that is the bias of the system,” the toxicologist said. “It’s like: Here’s someone that was found in a tent, we can’t contact their next of kin, we did a [urine drug screen]. They’ve got meth in their system; keep it moving. We’re not going to do an autopsy.”
Chronic meth use is definitely hard on your heart. So is sleeping outside. So is prison. So is poverty. The systems that were impacting someone on the day they died often leave signs we can physically see, but we don’t single out any of them to put on the death certificate; we do with meth, though.
A 30-year-old whose external autopsy shows meth in their system, even relatively low levels, is going to get logged as a meth death. If there’s fentanyl and meth, it’s a fent-meth death. This can still be the case once people get into their 50s and 60s, even though the odds of an underlying biological cause are much higher. Besides, if a body found in a tent does suggest heart failure or kidney failure or anything else with a correlation to meth, which could be pretty much any physical ailment experienced by the millions of people in the US who use meth, no one who formed their opinion of meth by reading about it is really going to question the cause.
There are a few approaches to how we improve the nation’s death data. One is to hope that medical students accumulating hundreds of thousands of dollars in debt are doing it so they can take an underpaid government job where all their patients are dead. Another is to decriminalize meth and all other illicit drugs. Forensic pathologists are often unavailable because they got pulled away to testify in court for something involving their toxicology analysis. Without jail or prison as an outcome, police don’t bother sending nearly as many samples to the lab, leaving pathologists free to keep on doing death investigations.
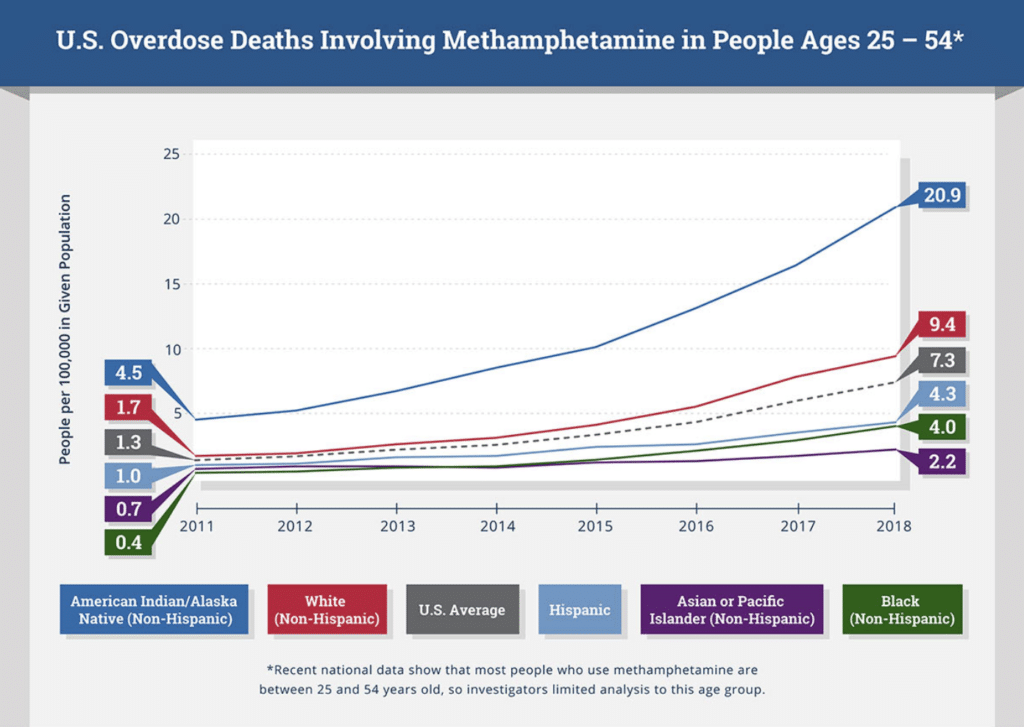
Top image via San Diego Office of Assessor, Recorder and County Clerk. Inset graphic via National Institutes of Health.





Show Comments