Early in the COVID-19 pandemic, in April 2020, there was a confirmed case at a pop-up shelter in Halifax, Nova Scotia. The unhoused residents—initially around 35 people, including some of the city’s most marginalized people who use drugs—were then moved into a fancy hotel in the city center to isolate.
Everything was such a mess at the time, much like it still is now. But a group of caring health care practitioners, including doctors, nurses, pharmacists, researchers, and harm reduction workers, took on the task of providing a safe supply of drugs to the people forced into the hotel.
Dr. Tommy Brothers, a resident physician training in general internal medicine and addiction medicine at Dalhousie University in Halifax, was one of them. He knew something had to be done—and done quickly.
“People could be at higher risk of overdose death if they were using an unsafe supply in their isolation hotel rooms.”
“When COVID-19 hit Halifax’s shelter system, we worried about how our patients and community members who use drugs and experience homelessness would be able to safely isolate or quarantine.” he told Filter. “We were facing a situation where people could be at higher risk of overdose death if they were using an unsafe supply in their isolation hotel rooms, or facing steep fines and criminalization if they had to leave.”
And what do you know? When you give people a safe place to live with regulated drugs, everything works out just fine.
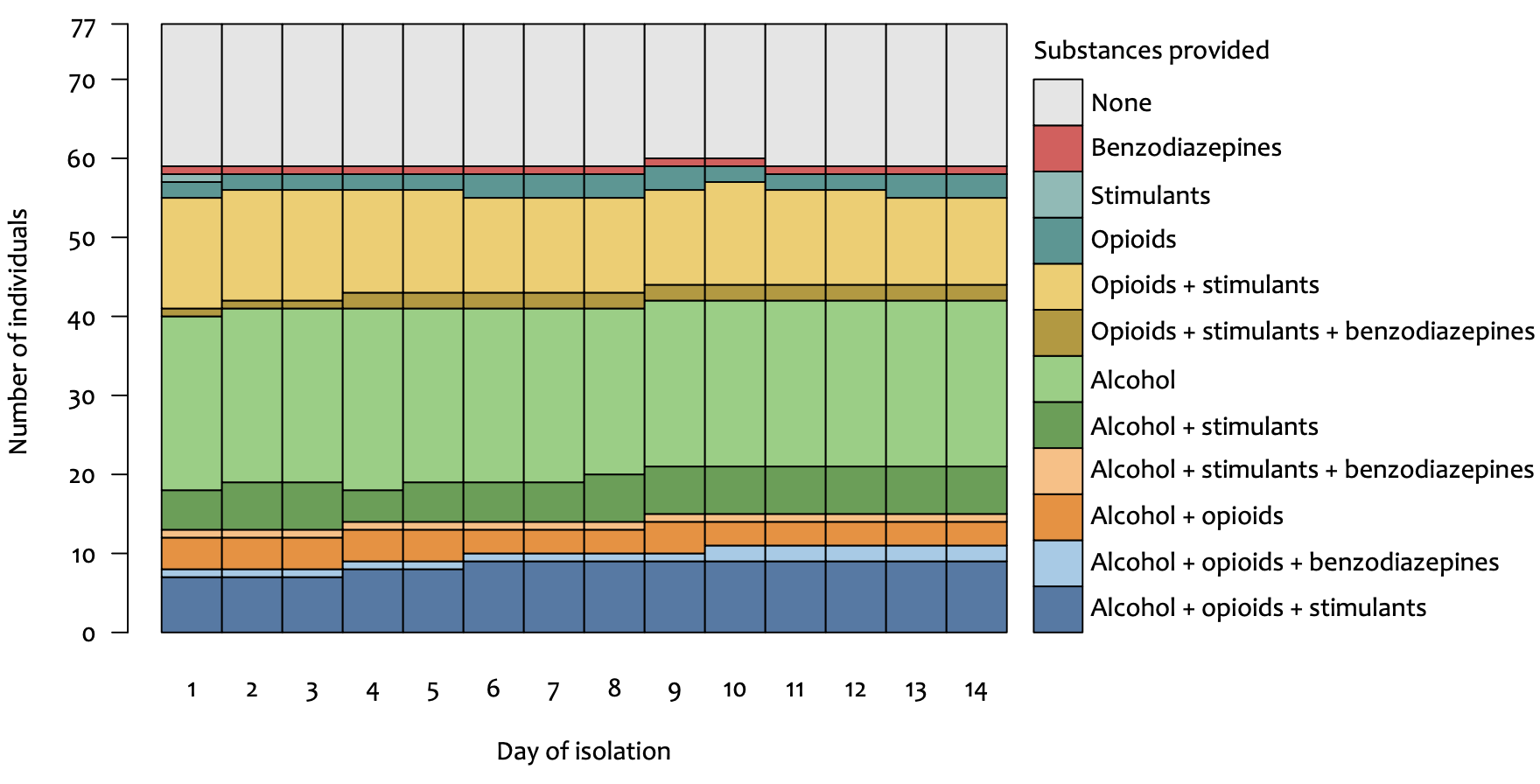
Over a period of 25 days, a total of 77 people were assessed, and 62 of them received assistance through this program. The supplies weren’t limited to pharmaceutical replacements for illegal drugs. People were also offered medicine, alcohol and even cigarettes. Essentially doctors asked their patients what they needed to isolate over that period, pharmacists prepared and delivered it and people used their drugs safely.
Most patients received various forms of opioid agonist therapy, but a lot received hydromorphone as well. Multiple patients were offered Dilaudid (short-acting hydromorphone) as a safe supply of opioids to inject, snort or consume orally.
People who used stimulants were given a variety of options for different forms of ADHD medication that could safely be used off-label. Nicotine users were provided with the means to avoid withdrawal that can have a range of negative mental health symptoms. And people who consumed alcohol—bearing in mind that sudden withdrawal can be dangerous and even life-threatening for heavy drinkers—were offered a variety of beer, wine or hard liquor.
Safe supply isn’t a very new concept—and it certainly wasn’t new to Dr. Brothers. His many mentors along the way have included Dr. Leah Genge, who has advocated for the introduction of safe supply throughout Nova Scotia. But there’s still a lot of doctors against it, apparently with no idea of how serious our crisis of drug poisoning is. It’s time for them to change their ways of practicing.
Taking care of this population in a pandemic isn’t easy, as I know all too well. I’ve been an avid fentanyl user for the past 10 years, and have overdosed twice during COVID; I was fortunate that people were on hand to administer naloxone and rescue breathing, and call for help.
But there was a strong will to get this right. “We have a really supportive community of harm reduction-oriented addiction medicine physicians, nurse practitioners, registered nurses, pharmacists, students and everyone in Halifax, and many were willing to volunteer their time to support people isolating in the hotel isolation shelters,” Brothers said.
“We were seeing firsthand the positive outcomes when people have safe housing, they have their substance-related needs met.”
While six people left isolation prematurely, four of those residents returned. And across the 1,059 combined nights people stayed at hotels later added to the program, there were zero overdoses. It was a stunning microcosm of how effective safe supply can be.
“We were seeing firsthand the positive outcomes that happen when people have their own safe and private housing, they have their substance-related needs met,” Brothers said.
But the city doesn’t seem to have fully learned the lessons of this success.
“Unfortunately as the pandemic has worn on, now only people who test positive for COVID are supported to isolate in hotels,” Brothers explained. “This means that there is less community in the hotels, and less peer support. I wish there were more resources to offer people more social and psychological support during these scary and lonely times.”
“The other thing I wish we could do differently is to give people the option to stay both in hotel housing and stay on safe supply long-term if they feel they are benefiting,” he added.
Put simply, people need an accessible, sustainable and regulated supply or they will continue to die.
The experiences in the isolation hotels have been documented for an original research paper by Brothers and his colleagues, to which I also contributed. The paper is currently going through a peer-review process to be accepted in an academic journal but the raw draft is already published.
It’s to be hoped that this will encourage a new, better way of practicing for marginalized drug users with complex needs. Put simply, people need an accessible, sustainable and regulated supply or they will continue to die. But if it wasn’t for Dr. Brothers and his compassionate colleagues stepping up at a time of crisis, things would have been far worse in our city.
Top photograph by Tommy Brothers. Inset chart from the draft paper.





Show Comments