There is no shortage of articles offering advice for how to deal with lockdown: Stick to a routine; get enough sleep; eat regular meals; maintain social connections (at a safe distance); and so on. Drug use often doesn’t make the list, but early signs suggest this is how many people are grappling with a dark and uncertain reality.
Market trends show that alcohol sales are up, though this could reflect stockpiling, especially in states that have closed or restricted liquor stores, or that people who were drinking in bars and restaurants are now doing it at home. A recent survey of over 2,000 people in the UK found diverging trends in alcohol consumption, with one-third of respondents reporting less frequent drinking and one-fifth reporting more frequent drinking since social distancing measures took effect. People who were drinking more often before the lockdown showed a greater tendency to continue or increase consumption compared to those who were drinking once a week or less—suggesting that one’s mid-pandemic drinking is influenced by one’s pre-pandemic drinking.
As for illicit drugs, anecdotal evidence and my own informal research suggest that people who were using before the coronavirus outbreak are continuing to do so, with some regular users having upped their intake.
It will be vital to keep track of substance use patterns as COVID-19 progresses. For now, we can reasonably assume that at least some people are using drugs, or using them more often, to cope with life’s new challenges: concern that oneself or loved ones will contract the virus, upending of normal work and social routines, financial instability, social isolation and loneliness, to name a few.
Understanding Why People Use Drugs
That drug use is a reaction to external stress may sound obvious, but the American response to drug use has rarely addressed environmental causes, instead treating it, at different points in time, as a moral failing or a chronic disease.
The currently prevailing view of drug use and addiction emphasizes biology over life events. According to the disease model of addiction, repetitive and prolonged drug use “hijacks” the brain’s reward system, leaving the person powerless over cravings. It is considered a chronic illness, often likened to such ailments as diabetes and hypertension.
While these analogies have helped gain support for medication-assisted treatment for opioid use or relatively less punitive drug policies, the disease model does not adequately account for the external context influencing a person’s drug use behavior—nor can it explain why people respond to drugs differently in different settings, or why most drug use never progresses to addiction.
All drugs, not just the ones people enjoy taking, can have adverse physical and neurological effects, but social and environmental factors are more relevant to understanding addiction and developing effective interventions.
Addiction to substances or behaviors is how some people adapt to this social dislocation.
Many addiction researchers, such as Carl Hart, Stanton Peele and Maia Szalavitz, among others, have laid out persuasive alternatives for explaining addiction that focus on an individual’s adaptive response to their environment. Bruce Alexander, who conducted the famous Rat Park experiments of the 1970s and ‘80s—which found that rats removed from social isolation and given toys and rat friends to play with were less interested in self-administered morphine—argues convincingly that a major underlying cause of addiction is the “breaking of social links that give people a sense of belonging, meaning, and identity.”
Addiction to substances or behaviors (gambling, shopping, sex, etc.) is how some people adapt to this social dislocation. It is experienced by both rich and poor, though people who face economic hardships are more likely to suffer from social ones as well.
The pandemic is worsening economic and psychological pressures. These problems are not experienced equally, of course, as underprivileged people are more vulnerable to the numerous and compounding tolls of COVID-19 and our response to it, and people will adapt in different ways. But uncertainty and anxiety are now central features of daily life for hundreds of millions of people in a way that they never were before.
A collective trauma of this magnitude may provide a clearer understanding of why people use drugs—to help us see it not as a moral failing or a malfunction of the brain’s risk and reward system, but as a fundamentally human response to negative life events.
Predicting Addiction in the Wake of the Pandemic
Whether an increase in pandemic-induced drug use translates into higher rates of addiction likely depends on the extent of the damage caused by COVID-19. But the outcomes will be instructive.
If we soon figure out how to resume economic and social activity without causing deadly surges in virus cases, and people are able to return to some degree of normalcy in a way that prevents long-term economic devastation, then it seems unlikely that COVID-19 will cause a large increase in addiction.
We can be relatively confident in this prediction because the vast majority of people who use substances, including drugs like heroin and meth that are often assumed to be especially addictive, do not develop substance use disorders (SUDs). Those who do develop SUDs typically recover on their own, without outside intervention.
The case of American soldiers in Vietnam who reported becoming addicted to heroin while overseas but ceased or vastly reduced their use after returning home (remission from addiction was an estimated 95 percent), demonstrates clearly that “addiction is a product of life circumstances.” If the conditions that caused a spike in a person’s drug use subside, that use is likely to diminish as well.
The risk will be most acute among people at society’s margins. The pandemic threatens to widen these margins.
But a quick recovery from the pandemic is far from certain. The more harmful and long-lasting the impact, the greater the risk that people using drugs to cope will continue to use, with little incentive to stop.
This risk will be most acute among people at society’s margins—people living in or near poverty, experiencing varying degrees of mental illness, with little or no healthcare, and few prospects for improving on these conditions. The pandemic threatens to widen these margins.
Changing the Narrative to Change the Response
By exacerbating conditions that cause people to use substances as a coping mechanism, and by making these conditions felt by many more people, COVID-19 has fostered greater urgency and opportunity to improve our understanding of drug use. How a problem is framed determines the kinds of solutions that people find acceptable, and recognizing addiction as an adaptive response is central to gaining support and funding for interventions tailored to a person’s underlying needs (housing, income, stability, physical and mental healthcare, etc.) and not solely or primarily their drug use.
While it is critical to highlight the environmental factors that contribute to problematic drug use and dependence, it is just as important to emphasize that non-problematic use is the norm, and that people use drugs for a variety of reasons (pain relief, emotional regulation, pleasure) without progressing to addiction.
Talking about, and normalizing, non-problematic use is essential.
Nuanced messaging doesn’t make for strong sound bites, and concerns about preventing addiction and drug-involved deaths have led us to neglect the complexity of drug use and intersecting issues. But talking about, and “normalizing,” non-problematic use is essential if we’re to reduce the persistent stigma that obstructs our ability to craft and implement more humane, equitable and effective drug policies.
In contrast, most reactions from the medical and health community to the real and potential increases in drug use mid-pandemic have come in the form of warnings—like this well-meaning PSA—that such use increases susceptibility to both COVID-19 and addiction.
Such messages, to the extent that they are accurate, may be important. But we should simultaneously acknowledge the ordinariness of substance use in response to hard times and offer people support for managing their use.
People who use drugs often engage in self-regulation and risk management strategies, including monitoring use patterns, setting limits on quantities consumed, and only using under certain conditions (with certain people, in a particular location, with a specific mindset or intent). Harm reduction groups have long argued for interventions that support and encourage self-regulation as a method of reducing risks associated with drug use. This skillset seems particularly relevant in the face of external stressors such as COVID-19, and can reduce the likelihood that people will develop problematic use patterns. Harm reductionists are discussing self-regulation strategies; this message should also be part of the mainstream conversation about life during the pandemic.
Normalizing drug use is critical to dismantling stigma towards people who use drugs—and to garnering public and financial support for the types of harm reduction and treatment interventions that are already sorely needed, and which are likely to be in higher demand in at least the immediate future.
The collective experience and trauma of COVID-19 should make it impossible to ignore the environmental context in which drug use takes place and that—despite the tragic nature of this learning opportunity—should invite progress.
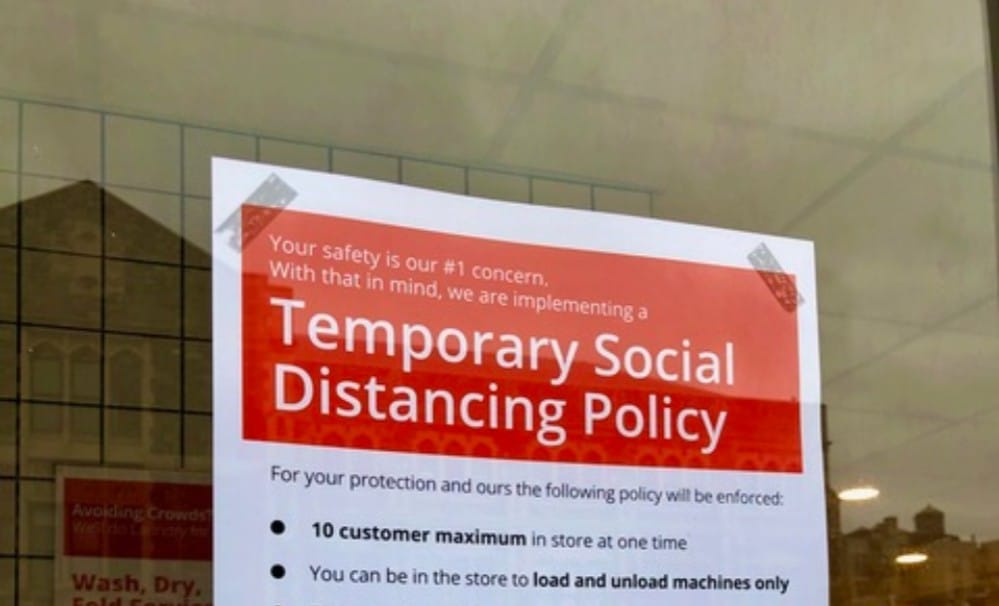
Photograph by Helen Redmond