In 2020, Ronald Richardson and his friends who used drugs in Philadelphia began noticing wounds forming on their bodies. This is now more widely known as a side effect of xylazine in the drug supply. At the time, Richardson didn’t understand why he had wounds because he didn’t inject drugs. So he went to his local emergency department.
“[The doctor] laughed me off,” he told Filter. “The doctor said he had been seeing patients for over 20 years and knows an IV user when he sees one. If I was any other patient there for any other reason, I think I would have been trusted more … I left even more afraid because, at that time, the doctors didn’t even know what was happening to me.”
This experience is one of countless that have harmfully impacted people who use drugs and their willingness to enter a hospital for services.
The emergency department is the entry point to care for so many folks who are not connected to traditional health care services. People who use drugs and other marginalized populations are subjected to many systematic harms. The breakdown of trust is one consequence.
If health care workers are not creating a safe space at the gate, the chances of a person returning or staying alive are sacrificed.
“As a Black man from West Philadelphia, certain things get propagated into our communities. For us, it was Suboxone clinics,” said Richardson, who no longer uses illicit drugs and is a certified recovery specialist working with peers and families. “It’s hard to trust what the medication can do when no one has ever taken the time to explain how it works. You can’t help but feel that you are lumped into a general demographic—how can trust build from that?”
If health care workers are not creating a safe space at the gate, the chances of a person returning or staying alive are sacrificed.
For the last three years, I have worked in the acute care setting in an emergency department in West Philadelphia. I have grown to love this community, and credit so much of my learning to my patients, who help me better understand both their needs and their perspectives.
I was hired to lead opioid use research in the department in 2020, just as the COVID-19 pandemic began to hit the United States. This position offered me a unique opportunity to fulfill my job tasks of clinical research while simultaneously being an advocate for patient-directed needs.
It was at that point I learned that there was culture change happening across the care spectrum. I also learned that progress was slow, at best. Yet I was able to find allies in the department to help support day-to-day change.
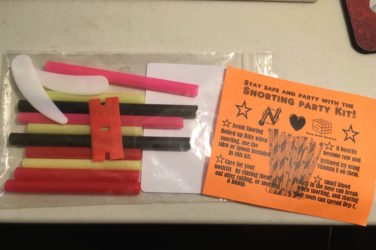
My team makes a point to meet folks at the door when we know they are coming in, so as to not have them go through security alone: an often-traumatizing experience, especially for people who have been impacted by the carceral system. Whether we are holding a patient’s hand while the tech searches for a vein or we’re equipping them with harm reduction kits, we fully recognize that rebuilding patients’ trust and having them feel supported is critical for their wellness.
Rachel McFadden, a nurse in both the emergency department and a wound-care clinic at a Philadelphia-based harm reduction organization, has been a clinical champion of shifting hospital culture when it comes to caring for people who use drugs.
Language is a great place to start when trying to remove stigma, and McFadden saw an opportunity to promote person-first language training for nurses in the emergency department. Her initiative has now fostered a small but positive change for the patients it serves.
Stand-out programs throughout the country are also pioneering necessary harm reduction interventions in health care settings—such as providing safer-use supplies, as we do in our own department.
Northern Inyo Healthcare District in California is a great example, thanks to former lead advocates Arlene Sun and Steven Dondero, who encouraged hospital-based syringe service programs (SSP). The pair also co-founded Skoden Native Harm Reduction Services under Crossroads Recovery Services, the first SSP tailored for Indigenous people in California. They now consult with other health care systems on how to bridge harm reduction and substance-use navigation gaps in clinical settings.
This interaction often sparks a deeper conversation about why the more compassionate reaction didn’t come naturally to the colleague at first.
McFadden’s work in West Philadelphia is informed by her recollection of receiving little-to-no real training in substance use or harm reduction during nursing school 10 years ago. She’s observed a slight curriculum shift since then; the same institution now offers special seminars on opioid use disorder, led by faculty who are experienced in substance-use care and harm reduction. But this is not a mandated course. Nor are such training opportunities standardized across all nursing programs in the country.
Additionally, while physicians are often expected to continuously take on new knowledge and evidence—via conferences, and grand rounds where colleagues share experiences and innovations—these expectations and opportunities often aren’t applied to the nursing community.
This gap, McFadden believes, places an onus on teaching at the bedside—in a way that meets both the nurse/provider and the patient where they’re at.
“When I interact with a colleague who is struggling with their feelings towards a person, I approach the patient the way I normally would,” she told Filter. “And then later that care provider comes back and says, ‘I really appreciated how nice you were to that patient.’”
This interaction often sparks a deeper conversation about why the more compassionate reaction didn’t come naturally to the colleague at first. McFadden’s example of care in a high-stress setting, she finds, can shift colleagues’ approaches going forward, leading to better experiences and outcomes for patients.
McFadden promotes peers in the clinical space, but emphasizes that their role does not remove individual accountability for other health care workers.
Having peer recovery specialists in the clinical setting has been another key strategy in supporting culture change and better outcomes. Peers can offer insights and connections to patients that no one without that experience really can; their place in this work is invaluable.
McFadden promotes peers in the clinical space, but emphasizes that their role does not remove individual accountability for other health care workers.
“Health systems and clinicians often place the heavy emotional work on a peer, instead of taking on that work themselves,” she noted.
But she added that shifting attitudes about people who use drugs “is a self-work project for a lot of people,” and that “we all have personal work to do to overcome our biases and judgments.”
“Meeting people where they’re at,” means doing exactly that for people who use drugs, of course. But it also applies to the work to challenge health-care stigma that McFadden, I and many others are doing. Self-righteousness isn’t a win; it pushes people away into shame, and shame doesn’t lead to good outcomes. So positive examples, encouragement, listening and constructive education are the path we choose. Creating a safe space where a teaching moment is possible is key.
Photograph by Brittany Salerno




Show Comments