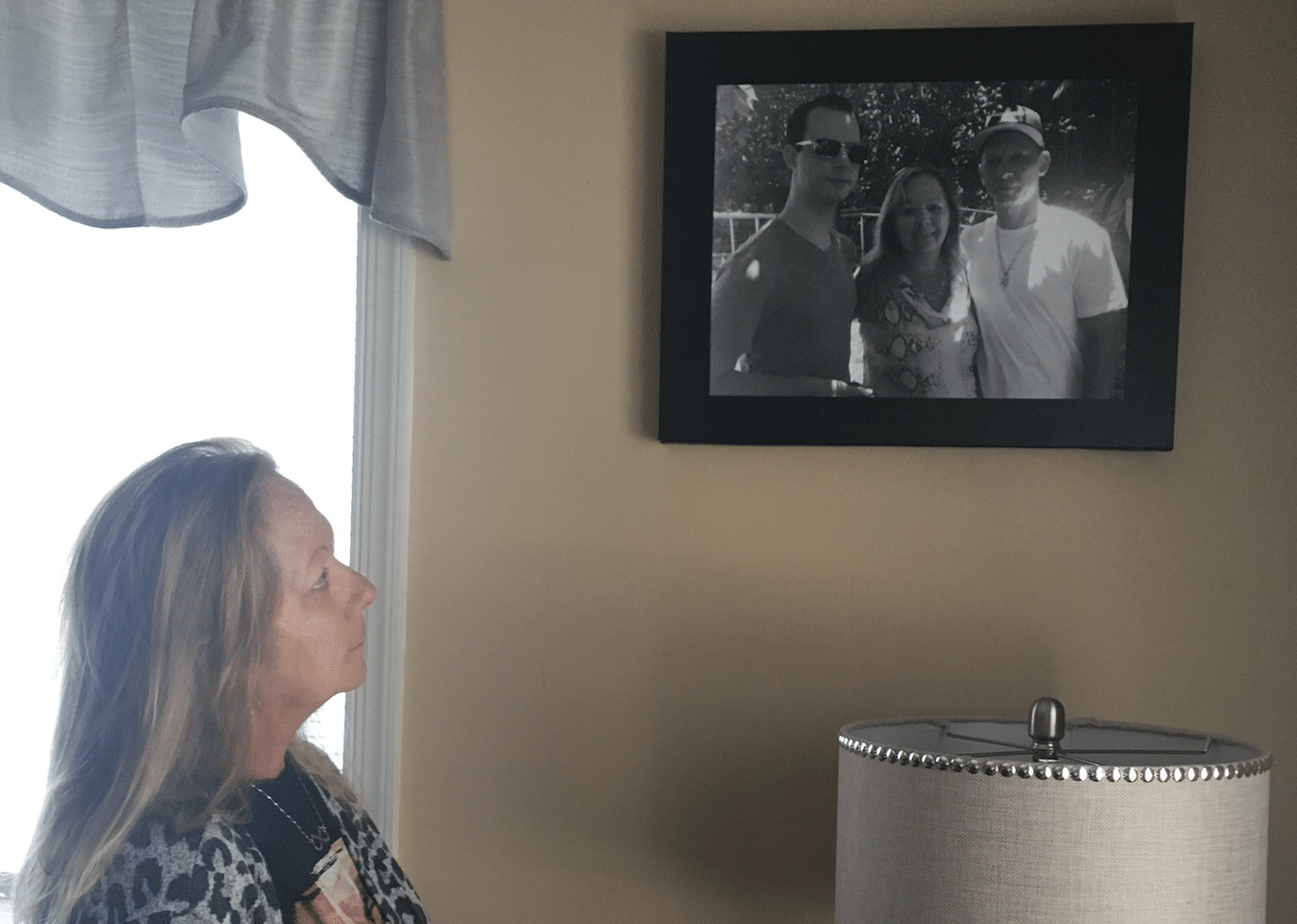
Dawn Troutt, of Delaware County, Pennsylvania, lost her 38-year-old son to a fentanyl-involved overdose on July 22, 2019.
Her son, Raymond Bauer, had experienced addiction and spells of recovery for years after his biological father took his own life in 2010. Unlike most people who are prescribed opioids, Bauer initially became addicted, as he described it, to the painkiller Percocet after having his wisdom teeth pulled. He then began using other opioids. A long cycle in and out of treatment began.
At various times, his journey involved recovery houses—residences where people who wish to abstain from drugs stay, often for months, typically following treatment for substance use disorder.
The person who was with him did not use naloxone. Troutt did not know whether naloxone was even available in the house.
At the last recovery house he lived in, in Philadelphia, residents used and sold drugs, Troutt said. There was very little oversight or structure, she continued, but the owner collected weekly rent and took food stamps from residents who received them. According to Troutt, the owner also coerced Bauer into going to doctors to try to get prescriptions for Wellbutrin, Adderall and Gabapentin, which the owner would then sell.
It was while living here that Bauer overdosed. The person (not an employee) who was with him at the time did not use naloxone, the opioid-overdose reversal drug, and called an ambulance only after videoing her son, Troutt said. She did not know whether naloxone was even available in the house—an egregious failing if it was not.
Troutt was furious to learn—in part through obtaining her son’s phone after he died—how the house was run.
Abstinence isn’t the only path to recovery from addiction—and for people with opioid use disorder, medications like methadone and buprenorphine are proven to greatly reduce mortality. But the point was, Bauer wished to remain abstinent, Troutt said, and he had chosen to live in a structured environment where abstinence was expected and supported. If this recovery house had operated as advertised, Troutt believes her son would still be alive today.
 Raymond Bauer in front of Philadelphia City Hall
Raymond Bauer in front of Philadelphia City Hall
Assuming that recovery houses were obliged to follow certain rules, she contacted some state politicians. “They just don’t want to do anything,” Troutt told Filter. “I called Harrisburg, and they said they [recovery houses] were privately owned so there was nothing they could do.”
The fact is, recovery houses (also known as sober living homes) are largely unregulated in many states.
“Some people [running recovery houses] do the best they can,” David Sheridan, executive director of the National Alliance for Recovery Residences (NARR), told Filter. “Unfortunately, there are all kinds of ways to do things badly.”
These include failing to provide and use naloxone, which NARR calls for.
“Basically, anyone with an unlicensed house can hang up a shingle and call it a recovery home.”
Part of the problem stems from the fact that the Affordable Care Act will pay for certain kinds of treatment but not for housing of this kind, Sheridan said. States can impose licensure regulations for homes that seek public funds, or that accept patients whose treatment is paid fully or partly by public funds. But even in states that do this, individual owners can choose to accept only private-pay clients, in which case they are not required to obtain a license.
And states cannot simply close down unlicensed houses because doing so would violate the Federal Fair Housing Act and Americans with Disabilities Act. “It’s a violation of the Fair Housing Act to impose conditions against people who chose to live together in support of their addiction like any other group,” Sheridan explained. “So basically, anyone with an unlicensed house can hang up a shingle and call it a recovery home, even if they fail to practice certain standards and NARR guidelines.”
This situation has led to many instances of exploitation, abuse and neglect at recovery homes around the country.
In 2014, Pennsylvania began the process of instituting a licensure program following recommendations from PARR, the local NARR chapter. This took effect December, 2021. To get a license from the state Department of Drug and Alcohol Programs (DDAP), owners need to write policies to protect residents’ rights, maintain records of payments, and complete state police criminal background checks for all staff and volunteers, among other requirements. Critically, licensed recovery houses must stock naloxone.
So far, two houses are licensed, 74 are in some stage of completing the application, and 26 are under review by DDAP’s licensing division, according to DDAP Policy Director Jordan Lewis.
“We hope that these regulations are giving residents and families of loved ones peace of mind that they’re living in a safe and supportive environment,” Lewis told Filter.
The licensure process wasn’t instituted until approximately a year-and-a-half after Bauer died. And again, owners who do not want to obtain a state license do not have to, but then give up the right to receive public funds, accept clients whose treatment is publicly funded, or house residents coming from treatment facilities that receive public funds.
Applicants for state licenses must allow residents to use FDA-approved opioid use disorder medications, which many facilities currently do not.
Last month, DDAP and Pennsylvania’s department of Community and Economic Development announced $1 million in grant funding for recovery houses seeking state licenses. The grants will help existing facilities with physical upgrades and inspections to comply with all federal, state, and local laws and ordinances. In the year beginning July 1, 2022, the state will award grants to between 22 and 25 eligible applicants. Applicants for state licenses must follow a series of requirements—including allowing residents to use FDA-approved opioid use disorder medications, which many facilities currently do not.
Sydney* spent years struggling with addiction and homelessness, sometimes engaging in sex work to buy drugs. She has identified as sober for the past three years. She told Filter that she was subjected to a corrupt, dirty and unregulated recovery home in Philadelphia. At one point, six inches of sewage flooded the basement. The kitchen was condemned for a time, so residents had to eat out for every meal, which was expensive. With little oversight, she said, residents were using drugs despite other residents having moved there because they wanted not to be around drug use.
“We need not to be looked at as scum coming off the street, and we need not to be living in sub-par housing,” Sydney said.
Worst of all, her best friend fatally overdosed in one of the facilities’ bedrooms last year. According to Sydney, naloxone either was not kept at the house or residents did not know where to find it.
In response to such problems in the city, concerned recovery home owners, people who work in the treatment community and people with lived experience have created a committee known as Harmful Ethics Reduction (HER). The group maintains a list of reputable recovery homes and those for which it has received complaints. Residents can report issues directly to HER.
Another recovery house owner-operator told Filter he has lost two residents over the years to fentanyl-involved overdoses.
The main goal is not to close down corrupt or unsupervised recovery houses, but rather to offer owners ways to improve, including help in areas such as naloxone training and proper oversight, said Sarah Laurel, a founding HER member, who also runs Savage Sisters with her brother. The nonprofit operates five recovery houses and provides harm reduction outreach, as well as programming to support people who choose abstinence. Savage Sisters is in the process of applying for a state license.
Another recovery house owner-operator, Andre DeFrancesco of Franklin Recovery Sober Living Home, has been running a series of homes in Philadelphia since 2015. DeFrancesco told Filter he has lost two residents over the years to fentanyl-involved overdoses. One was four years ago, when his homes did not have naloxone. The other was a year-and-a-half ago, when naloxone was present but the person was alone when he died.
DeFrancesco, who is currently going through the state licensure process and refurbishing his facilities, admitted that running recovery housing has been a learning curve. He said that he deeply regrets the two deaths.
“Now there’s Narcan all over the place,” he said, adding that all staff and residents must have naloxone training.
States that have instituted more robust regulations include Florida, which has involved NARR in a state task force to do so. The regulations include providing a physically and emotionally safe, secure and respectful environment with naloxone on hand; maintaining a record of all residents’ charges, payments and deposits; documenting that residents participate in developing their own recovery plans; and providing a clear structure of written and enforced policies, among other requirements.
“Other states that have really come around are some of the surprising ones, such as Kentucky and West Virginia,” Sheridan said. Oklahoma has also done well, he added, by fully funding the local NARR chapter, helping underwrite the cost of certification, providing free training for operators and peer staff, and offering vouchers to counties to incentivize people to open regulated recovery homes.
“The recovery house never called us to say she had died. We found out through her friends.”
Yet such examples remain the exception. There’s no comprehensive data on recovery houses because statistics are only available for facilities that seek certification in the approximately 15 states that actively license homes, according to NARR. “The number of homes that are not certified by this organization is unknown,” NARR’s website says. This leaves a wide gap for rogue actors to open homes and abuse clients.
Kiersten Eaton, of New Jersey, lost her sister, Ashley, to a fentanyl-involved overdose in a Philadelphia recovery house last year. “The recovery house never called us to say she had died,” Eaton said, crying. “We found out through her friends.”
Once again, residents did not know whether naloxone was kept at the house and if so, where it was.
After obtaining her sister’s phone, Eaton began to understand the extent of the other problems in the house—among them bedbugs, drug sales on the property and inadequate oversight.
“My dad says a parent is not supposed to bury their child,” Eaton said. “The amount of pain that you feel, even just on an everyday basis—it’s not that it even gets better. You just learn to live with the pain. I want to prevent other families from going through the same things.”
*Name changed to protect source’s privacy.
Correction, April 5: A quote from David Sheridan in the second half of this article was originally misattributed to Jordan Lewis. The article has been edited to correct this.
Photographs, including top photograph of Dawn Troutt, courtesy of Troutt.




Show Comments