On May 7, UNAIDS called for prisoner access to harm reduction—medication for opioid use disorder, sterile syringes and condoms—to reduce viral transmission of HIV, along with hepatitis C. I’m told that in the harm reduction movement outside of prison, when people talk about viral transmission they’re referring mainly to just those two. Which makes sense for the harm reduction work taking place out there, but in here the conversation isn’t about two viruses—it’s about four.
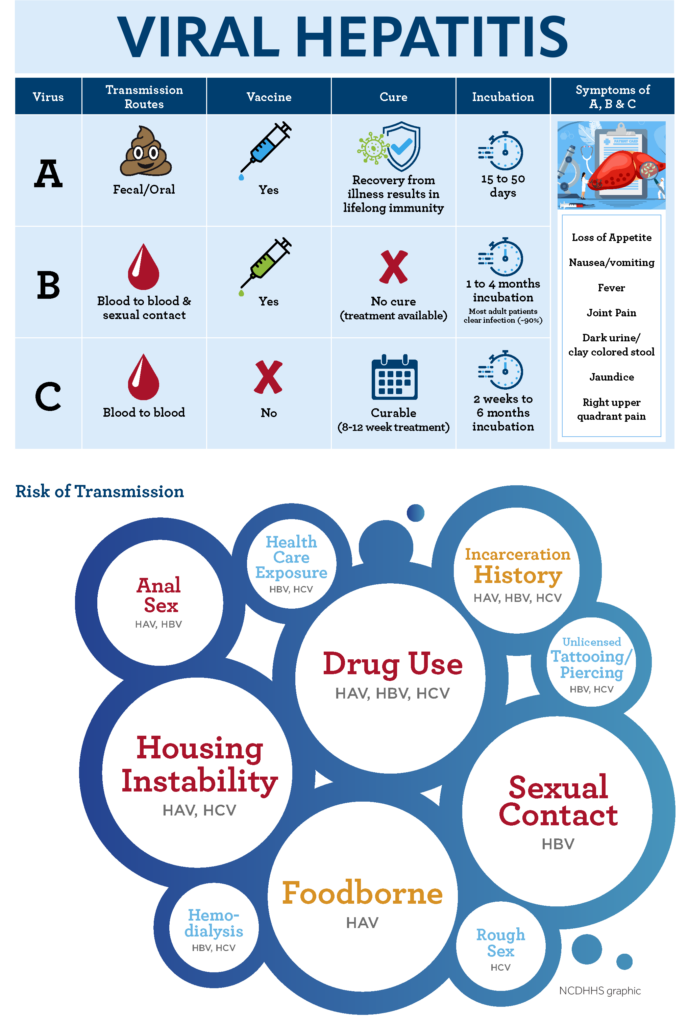
Hepatitis A and B are both found in the blood, as is the case with HIV and the virus that can lead to hep C (HCV). But the hep A virus (HAV) is also found in fecal matter, and the hep B virus (HBV) in various bodily fluids including semen. In the United States, this means hep A and B disproportionately impact people who use drugs, but also people who’ve lost access to housing or who do survival sex work—especially men who have sex with men. These are the same people disproportionately impacted by prison.
Hep A and B are the inverse of hep C when it comes to prevention and treatment: They have vaccines, but not cures. One of the most concrete forms of harm reduction for hep A and B here is making sure people know that if they access the vaccine through the infectious disease department, it’s free. The regular route requires a $4 copay, and many people here don’t have $4 on their account; those who do are going to put it toward a 3-ounce bag of instant coffee. Either way, no one’s going to get vaccinated.
Hep A is not considered much of a concern in the United States—if you forget the nearly 2 million people inside prisons and jails.
Beyond that, most hep A and B harm reduction here at Washington Corrections Center comes down to education. When I was diagnosed with HIV in 1992 and entered the state prison system not long after, everyone was terrified of sharing razors and needles, although of course they still did. Today, a lot of people here who pass through this prison think HIV is over, the way people think COVID-19 is over, and I have to remind them why it’s still important to avoid sharing razors and needles, and how to sterilize them if you do.
Hep A is an acute inflammation of the liver. It can make someone severely ill for months, but once it clears they’re immunized for life. HAV usually spreads through fecal matter: by way of anal sex, or by ingesting it—for example by eating food touched by someone who hasn’t washed their hands.
Because of this, it’s much more common in parts of the world where running water isn’t available, and not considered much of a concern in the United States—if you forget the nearly 2 million people inside the nation’s prisons and jails, where living conditions bear little resemblance to the outside. When people are locked in a place with shit smeared across the walls and not given any way to clean it, hep A prevalence is going to go up.
A lot of prisoners didn’t have stable housing, or any housing, before they were incarcerated. It’s often why they were incarcerated. Folks often enter prisons and jails at times in their life when they’re not in the habit of washing their hands. There’s not much in the way of hep A education here, and bringing it to people’s attention in a non-stigmatizing way actually has two functions: not only viral hepatitis harm reduction, but violence harm reduction.
Fights here regularly start when someone is seen leaving the bathroom and heading in the direction of the microwave. So discreetly talking to someone about how washing their hands reduces hep A transmission also reduces that person’s risk of getting punched in the head.
In prison, safer sex can mean unprotected sex; safer injection can mean flushing a syringe with just water, not bleach.
Hep B is a sexually transmitted infection (STI). Sex work in men’s prisons is common, but usually not safe to discuss.
We don’t have condoms, and people often think the plastic cling film used to wrap sandwiches is a good material for a makeshift version. But we only get the microwave-safe kind—it’s all perforated. Aside from being ineffective, it creates extra friction and potentially raises risk of blood-to-blood transmission. The safer option is no “condom,” as much lube as possible, and pull out.
To varying degrees, thoroughly flushing a syringe with bleach reduces risk of transmitting all viral hepatitis as well as HIV. That’s good harm reduction for situations where someone needs to reuse a syringe maybe a couple of times before they can get a new one. In prisons, syringes are reused as many times as possible. This means that keeping the needle sharp, and the overall rig intact, is more important than taking a gamble on sterilizing it.
Bleach degrades a syringe, especially if you do the full process necessary to have at least some chance of killing some viruses. Ragged needles and wobbly barrels make abscesses and bacterial infections become the more pressing concern. When you don’t have the $4 to go to medical, the safer option is to flush with water as many times as possible between each shot. The idea is that rather than trying to kill the viruses with bleach, you’re trying to remove leftover blood from the syringe, and any lingering virus along with it.
“The more you rinse the better,” reads the Self-Help in Eliminating Life-Threatening Diseases curriculum I use to teach blood-borne pathogen harm reduction. “Rinsing five times with cold water is great.”
cdc-hiv-consumer-info-sheet-cleaning-syringes
Talking to other prisoners about hep A and B has one more important function: It eases people into the conversation about hep C and HIV. If you start with those right off the bat, people will often come at you in anger or else just shut down.
Very few people in the US die of hep A each year. Around 3,000 die of hep B; the mortality rate among Asian Americans and Pacific Islanders is around nine times that of white people. We know more than 15,000 US deaths per year are attributed to hep C, and that mortality is disproportionately high in Indigenous and Black communities.
HIV prevalence inside US prisons is around three times higher than in the general population. For hep C it’s estimated to be around 20 times higher, but any numbers associated with HCV are widely acknowledged to be undercounts.
Dozens of countries have already begun implementing the harm reduction measures needed to change this. In Moldova, resources like methadone, sterile syringes, condoms and non-mandated counseling have been accessible in some prisons for more than two decades. The result has been a reduction of viral hepatitis, HIV, STI and injection infections, with no increase in drug use, or any discernible harms to either prisoners or staff. As of May 5, those resources have been expanded to every prison in the country.
I imagine that harm reduction in those facilities looks a bit more like it does in the free world, premised around distribution of a few critical supplies. In an environment without any of those supplies, harm reduction looks very different. Safer sex might mean unprotected sex; safer injection might mean reusing syringes without chemically disinfecting them. Of course, US prisons don’t have to be this way; the people in power choose for them to be this way.
Top image via Ohio Department of Health. Middle graphic via Cumberland County, North Carolina. Bottom graphic via Centers for Disease Control and Prevention





Show Comments