Conditions in the Kensington neighborhood of North Philadelphia, where I’ve reported for years, stand as a rebuke to a litany of drug policy failures. Over the past three decades city, state and federal officials have tried one enforcement-centered approach after another—stick, carrot and combinations of the two—to make a dent in Kensington’s thriving illicit drug economy. Yet drugs are today cheaper and found in greater variety than ever before—and people are dying in greater numbers.
Amid a wave of synthetic drugs in recent years, Kensington has emerged as the locus for a different kind of experimentation, through a new generation of freelance entrepreneurs. Their bathtub chemistry is often guided by trial and error—leaving doctors, public health officials and harm reductionists struggling to understand the latest side effects. Over the past 12 months alone, these have included palsy-like rigidity in the hands and arms of some drug users; an outbreak of necrotic skin lesions; and a rise in the number of people who inject drugs losing consciousness, or wandering into traffic in a state of semi-consciousness.
Last year, a concerned toxicologist from the nonprofit Center for Forensic Science Research & Education (CFSRE) at the Fredric Rieders Family Foundation, the academic and research arm of NMS Labs outside Philadelphia, conceived of a new testing program. It employs sophisticated mass spectrometry to reveal the composition of retail-level street drugs.
Alex Krotulski, an associate director of the CFSRE, says the ultimate goal is to predict the next poisoning outbreak before it happens.
“Through various surveillance and monitoring initiatives, paired with information about drug use habits and preferences, we decided it was vitally important to develop a program that could answer complex questions about drug use and trends by using accurate and reliable scientific data,” Krotulski told Filter.
The program, called NPS Discovery, deals with many aspects of drug use, markets and trends, but its reliance on real-time testing of street drug samples is what sets it apart. (Full disclosure: I was an unpaid adviser to the program during its inception and provided some early samples for testing.)
“Our program focuses … on timely information for rapid dissemination to all affected communities.”
Relatively few programs unrelated to law enforcement have both the will and the technology to fully analyze drug samples and compile data. The Dope Project, in the Bay Area of San Francisco, was a trailblazer when it began a sample testing program several years ago. The Urban Survivors Union in North Carolina recently acquired a mass spectrometer to decipher the ingredients of street drugs. Another program, supported by Brandeis University, exists in Massachusetts.
But most research on the evolution of synthetic drugs continues to rely on postmortem toxicology, or the results of tests taken in conjunction with civil or criminal court cases. Since these tests are focused on what happened in the past rather than taking a snapshot of the current market, they have little preventative value.
“The drug market remains a highly dynamic landscape … data and information from six months to a year ago is likely already out of date and not actionable in the current climate,” said Krotulski. “Our program focuses specifically on the acquisition of timely information for rapid dissemination to all affected communities.”
Krotulski’s mission bore fruit with the release of NPS Discovery’s revealing first report earlier this year. It’s a mission driven by Philadelphia’s recent experiences.
What Happens When We Don’t Know
Over the past several years, novel psychoactive substances (NPS)—a catch-all term used to describe countless synthetic variants of completely different drugs—have taken the United States by storm, in some cases all but displacing demand for their organic predecessors.
In 2000, when synthetic cannabinoids were first hitting US streets as an alternative to marijuana, young Kensington residents on probation particularly favored them. They were a means to avoid positives on drug tests that didn’t detect K2 or Spice, as some of the variants were branded.
Then came fentanyl. By around 2016, it had displaced heroin as the primary ingredient in Kensington heroin, as my own informal testing confirmed, among much other evidence. This cut the cost of a bag of “dope” in half, from $10 to just $5. People could now fix up for the price of a Starbucks latte. But the impact of uncertain dosages of the powerful synthetic on people who often didn’t know what they were using was deadly. In 2017, more than 1,200 people died in Philadelphia of drug overdoses—three times the previous average annual rate.
City health officials responded by flooding the streets with the overdose reversal drug naloxone. But in the summer and fall of 2018, a new drug concoction would test the limits of that strategy when many hundreds of people fell ill after injecting Kensington dope. In most cases naloxone didn’t seem to help—people who received it were experiencing unusual reactions and becoming severely agitated.
To Krotulski, the event revealed the limits of toxicology reports in deciphering Philadelphia’s increasingly Balkanized synthetic drug market.
Subsequent testing revealed the cause. Several brands of Philly dope had been mixed with a powerful synthetic cannabinoid. Not only was naloxone ineffective at reversing that drug’s effect, in some cases it made things worse—by blocking the sedating effects of any opioids in the mix, and leaving people experiencing the often-unfavorable hallucinogenic properties of the synthetic cannabinoid alone.
“I felt like I was trapped in a box and I couldn’t get out,” one middle-aged man told me in the weeks following the outbreak. “I thought I was gonna die. I never want to feel that way again.”
That situation lasted only a couple of months. But it demonstrated how harms follow when public health responses are two steps behind rapidly changing drug markets.
Krotulski helped to identify the key contaminant in that case: It was 5F-AFB, one of several hundred potent synthetic cannabinoid variants. To him, the event revealed the limits of toxicology reports in deciphering Philadelphia’s increasingly Balkanized synthetic drug market. And this inspired what became NPS Discovery.
“Before we investigated these cases of 5F-ADB and heroin/fentanyl, we understood the possibility of drug mixing and the implications of taking different psychoactive substances together, but we did not fully understand the downstream effects on drug users, clinical providers, laboratories, and many others,” Krotulski explained. “These circumstances stressed the need for investigating raw drug materials, as this was the only way we would understand the true nature of the drug supply and its potential harm.”
The Project’s First Findings
NPS Discovery has grown and now has many collaborators and partners, including Philadelphia’s Department of Public Health. In February, these organizations collectively released their first report.
The report illustrates a market in a state of constant flux—driven by drug laws, and the creative chemistry and marketing designed to circumvent them.
Nearly 100 drug samples were obtained and tested. While heroin is still present in some bags of Philly dope, as well as fentanyl and its analogs, the predominant ingredient has become xylazine—a non-opioid animal sedative whose emergence I reported on for Filter in 2019. Every single “heroin” sample tested positive for the drug, which can be readily obtained by anyone with a veterinary license.
Xaylazine—a vasoconstrictor that impairs blood flow to the extremities—is believed to be responsible for an outbreak of necrotic skin lesions around the injection sites of some people who use drugs. Researchers from the University of North Carolina told me they are concerned about xylazine causing dangerously low blood pressure, and are investigating a link with low red blood cell counts.
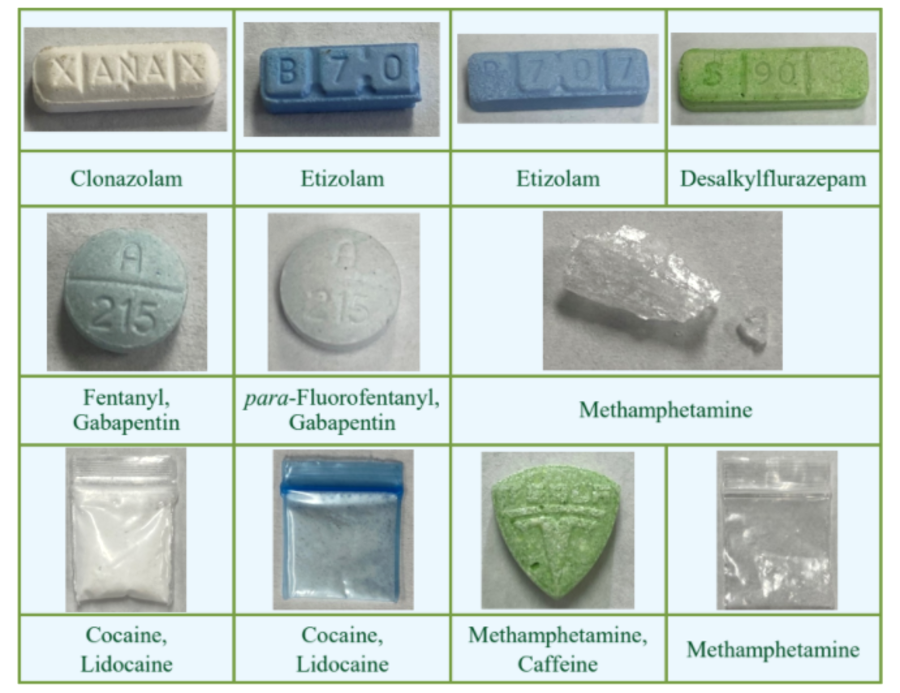
Counterfeit pills also remain an issue. In one case, a tablet sold as “ecstasy” turned out to be methamphetamine and caffeine. In another, a “generic oxycodone” tablet was revealed to contain no oxycodone at all, but rather was pressed with para-Fluorofentanyl—an analog that Krotulski said is believed to be synthesized in Mexico and is showing up in more powder and pill samples.
The white powder samples did indeed contain cocaine—typically cut with lidocaine, levamisole or caffeine.
In some cases the data showed improvements in market conditions, or else dispelled long-running myths about the composition of street drugs.
Powder cocaine, sold in Kensington in bags ranging from $5-$20, has been the subject of much conjecture among people who use it. “All this coke is junk,” Ana, my long-time fixer and translator has told me. “It’s got bath salts in it.” Dozens of other people have told me that much of Kensington’s coke is really composed of the plethora of cathinones colloquially known as “bath salts.”
However NPS Discovery’s mass spectrometry testing did not reveal a single cathinone. The white powder samples did indeed contain cocaine—typically cut with lidocaine, levamisole or caffeine.
Meanwhile, methamphetamine in Philly seems to be largely unadulterated, according to all of the samples tested. NPS Discovery is working on instituting quantitative mass spectrometry testing to determine drugs’ purity levels.
In one piece of good news, Krotulski’s report suggested that the deadly practice of pressing fentanyl into “benzodiazepine” pills (particularly “Xanax”) may be over in Philadelphia. None of the pills sold as Xanax that were tested showed up positive for fentanyl. Instead, pill pressers seem to have discovered the handful of unscheduled benzodiazepine analogs readily available in the research chemical market, including etizolam and flurazepam. In this case, supply-side innovation worked to the benefit of harm reduction, not against it.
The NPS Discovery program and others like it make clear, as if we needed a reminder, that prohibition has failed—miserably so. Economics will always beat bans. Drug suppliers don’t want to harm their clients, but negligence and inexperience will create harms when bad policies dictate the means of pursuing profits.
Our policies incentivize bad business practices, with no regulatory oversight. Product innovation, for example, seems to have eliminated the potential for someone to die of an opioid overdose in Philadelphia after taking what they believed to be Xanax. But I’d bet my last dollar that if pressed etizolam becomes more widespread, that will be pushed underground too.
It is hoped that more NPS Discovery reports, of increasing scope, will follow. It will be up to public health officials and harm reductionists to put their potentially lifesaving information to the best possible use.
For a deep dive into the findings of NPS Discovery’s first report, listen to Christopher Moraff’s upcoming interview with forensic toxicologist Alex Krotulski on the podcast Narcotica.




Show Comments