For months, media outlets including Filter have reported on a collage of anecdotal and local alerts from around the country that drug overdose deaths have been spiking since the COVID-19 pandemic began. On October 14, the federal Centers for Disease Control and Prevention (CDC) finally confirmed this development on a national scale with the release of preliminary data.
The data—which, again, are subject to change and not final—estimate how many drug overdoses happened in the US in the first three months of the year. Of course, the first US COVID-19 case was in January, and business closures and the government-ordered lockdowns followed in February and March. The CDC found that in that quarter, we lost over 19,400 lives to a drug overdose. That is an increase of over 16 percent, or nearly 3,000 more deaths, compared to the same period in 2019.
It seems clear that overdoses were increasing even before the pandemic, but rose faster after its onset. Here are some key insights from the CDC’s data:
* Drug overdoses increased by over 5,000 for the 12-month periods ending in both February and March 2020, reaching 72,000 and 74,000 deaths, respectively. These figures represent record high count for deaths, following two years of high-but-stable 12-month numbers. After peaking in November 2017, these death counts started declining—then started rising again from January 2019.
* Thirty-eight states and Washington, DC saw deaths go up, while the other states saw decreases. The sharpest spike was in South Dakota. The most populous US states, including California, Texas, Florida, and New York, all saw significant increases.
* The most common drug category involved in deaths remains opioids. But broken down further, it is clear that illicity synthetic opioids including fentanyl are responsible for most deaths. For drugs like heroin, prescription painkillers and methadone, overdose deaths are stable or even declining slowly.
* Deaths involving stimulants such as methamphetamine and cocaine are steadily increasing. This follows emerging trends that have been clear for years now. It must be noted that overdoses from stimulants are also tied to synthetic opioids. Most deaths involved drug combinations, and street meth and cocaine supplies, among others, have been adulterated with fentanyl and similar substances.
The CDC’s data confirm our fears that COVID-19 is exacerbating the drug overdose epidemic, said Dr. Jules Netherland, director of the Drug Policy Alliance’s Department of Research and Academic Engagement.*
“It is likely a combination of factors, including social isolation, disruptions in drug supply, and the difficulty of accessing harm reduction and treatment services.”
“While there is still little research on exactly how COVID-19 is contributing to an increase in overdose deaths, it is likely due to a combination of factors, including social isolation, disruptions in drug supply, and the difficulty of accessing harm reduction and treatment services,” Netherland told Filter. “It is also probable that people who use drugs are at increased risk for COVID-19, especially because they are more likely to face barriers to healthcare, underlying health conditions and poverty.”
Netherland emphasized that our response to the crisis must not overlook the rising deaths involving stimulants. “To address this, we need comprehensive harm reduction and treatment strategies that take into account the unique issues surrounding stimulant use,” she said. “Safe consumption spaces, harm reduction education and services tailored for stimulant users, and drug checking programs can all help reduce overdose deaths.”
Arash Diba, a harm reduction director for VOCAL-NY, agreed that the CDC data illustrate what he described as a “fatal recipe.”
“COVID-19 closed our drop-in centers, which was for some people the only social tether to safety and a welcoming community,” Diba told Filter. “When people would come in for needles, they would want to hang around. Now, more people are using alone, not having their safer spaces where they used before.”
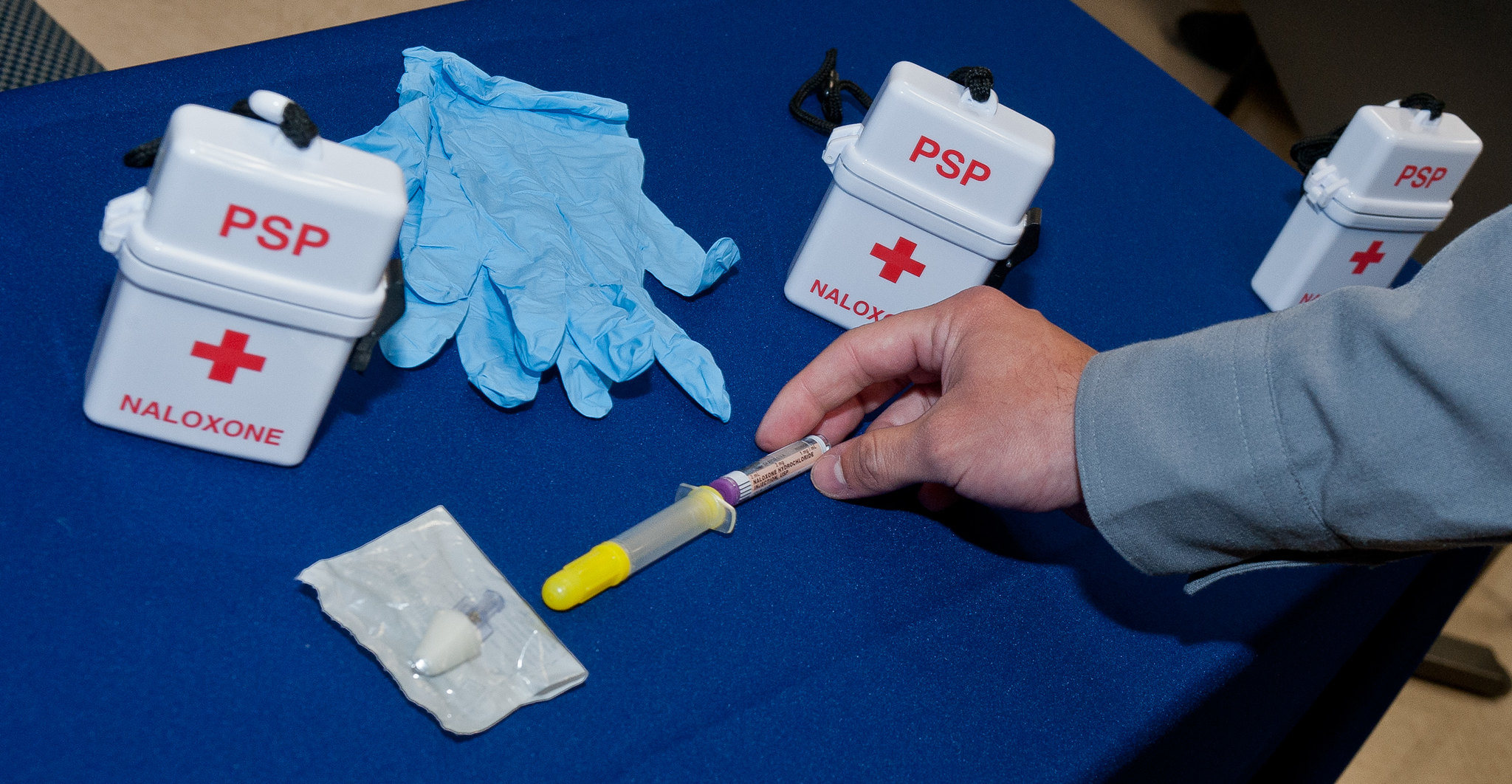
Having to use alone carries many risks. People may be impeded from sharing information with each other about the quality and purity of local drug supplies—especially as regards fentanyl. And if someone overdoses alone, no one will be able to administer fentanyl.
Global turmoil has also disrupted local drug supplies. Diba suspects that more fentanyl is now circulating, and is calling for a legal safe supply of drugs to provide an uncontaminated source.
“And many of us have been begging Governor Cuomo for years to green-light the Overdose Prevention Center pilot program he promised,” Diba added. “That would let drug users inject in a supervised, naloxone-ready setting, out of view of the public, at a time when available public bathrooms are locked down during COVID-19.”
But how do you prevent drug overdoses in a country where you are locked up for simple possession? How do you ensure care for vulnerable people when healthcare itself is a big business? The solutions have less to do with drugs, said Kristen Marshall, an overdose prevention specialist for the National Harm Reduction Coalition, and more to do with deeper systemic change.
“This is about racism and poverty; it’s about lack of access to sound medical and mental health care; it’s about trauma; it’s about health and economic disparities.”
Marshall explained that the people most at risk of drug overdose often tend to experience the greatest economic and health disparities in the US. “Isolation, the chaos of uncertainty, and overall despair are absolutely contributing factors to this year’s rise in overdose deaths,” she told Filter. “Even though we are all experiencing those things to some extent, the less resources someone has, isolation intensifies, uncertainty becomes more chaotic, and the despair becomes deeper. ”
“This is about people,” she continued, “and it’s about people who are systematically excluded from care and equity in our country. This is about racism and poverty; it’s about lack of access to sound medical and mental health care; it’s about trauma; it’s about health and economic disparities, and the fact that in this country, we exist under a system that says some people deserve care and resources, and some people don’t.”
Marshall’s insights are evident within the CDC data. Overdoses among white people actually declined slightly, while rising significantly for Black and Hispanic Americans. Filter has previously reported on the facts that Black Americans are now disproportionately likely to die of fentanyl-involved overdose and to be impacted by COVID-19.
By age, the largest increase in overdose deaths since the first quarter of 2019 was among people aged 14-24, and the next two age groups up to 44 years old saw larger increases than all others.
Marshall urged that we fight both drug overdoses and COVID-19 by ending the drug war and mass incarceration, ensuring housing for all, and working towards racial and economic justice. “All of these things can be written into policy, all of these things are actually achievable, and all of these things address the root of drug use and overdose,” she said.
*DPA has previously provided a restricted grant to The Influence Foundation, which operates Filter, to support a Drug War Journalism Diversity Fellowship.
Photo via Flickr/Creative Commons 2.0