What is the best way to protect more women who use drugs from HIV treatment? Researchers examined one aspect this question with a pilot study in Philadelphia in which they gave participating women PrEP, the HIV prevention regimen. They found that partnering with an established syringe service program (SSP) was an effective strategy.
The study focused on the Kensington neighborhood, which has experienced high overdose rates—as well as political battles over residents who use drugs or are homeless. The researchers partnered with Prevention Point Philadelphia, which has been the only authorized SSP in the city for nearly 30 years.
“Integrating clinical care into needed social services is a proven way to engage vulnerable and marginalized populations—like women who use drugs—in preventive health care and treatment,” first author Dr. Alexis Roth told Filter. Roth, an associate professor at Drexel University’s Dornsife School of Public Health, said that the researchers “benefited from the longstanding trust Prevention Point staff had garnered with their clients. Offering PrEP as part of their services was simply a new harm reduction tool that women could take advantage of.”
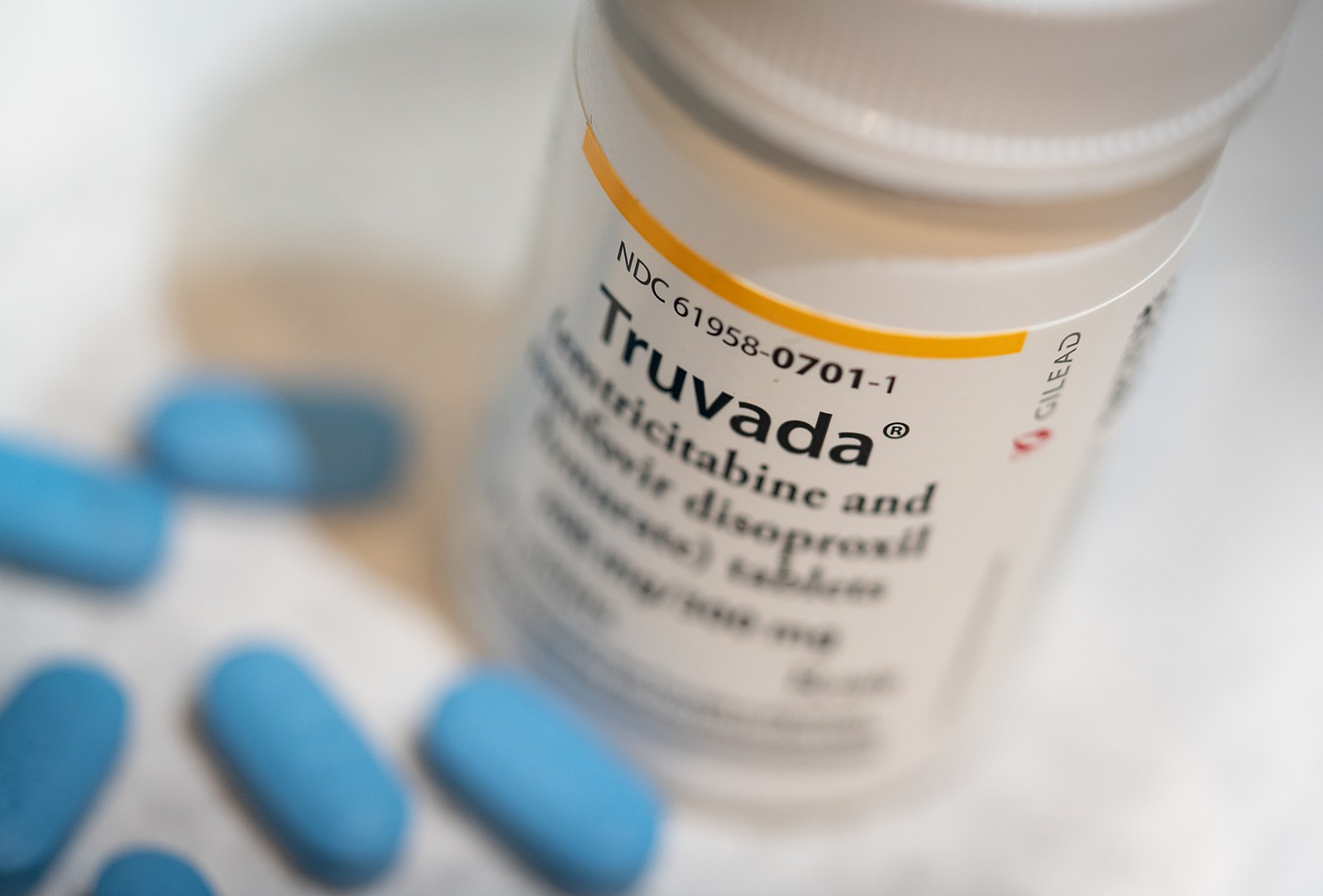
Pre-exposure prophylaxis (PrEP) is often understood to refer to medication, but also encompasses a range of harm reduction interventions—regular medical appointments, blood work, condom use, safer sex education, etc.—of which medication is one component. The PrEP medication chosen for this study, Truvada, is approved for patients with vaginal tissue (the other common PrEP medication, Descovy, is approved for rectal tissue).
Truvada works by blocking an enzyme that allows the HIV virus to replicate inside the body. The CDC estimates Truvada is about 90 percent effective for preventing HIV transmission from sex and 70 percent effective for preventing transmission from injection drug use. The researchers offered the women Truvada for 24 weeks, in addition to blood tests and medical counseling.
Roth’s team initially recruited over 130 adult women who inject drugs. All of the women were cisgender, and about two-thirds identified as homeless with an annual income of less than $5,000. They were predominantly non-Hispanic white.
“One of our next steps will to be to include trans women who inject drugs as well.”
These demographics show the study’s limitations, as transgender women are disproportionately impacted HIV and also understudied in its prevention. The study sample was also significantly whiter than the city’s population; participants volunteered themselves for the study.
“As a first step to increase access to PrEP for women who inject drugs, in Project SHE, we chose to specifically focus on cisgender women,” Roth said. “The [minimum] threshold for adherence to achieve maximum protective effects from PrEP is highest in this group … the issue is concentration of [medication] in the vagina compared to in the rectum.”
“Thus, our pilot focused on trying to understand their specific facilitators and barriers to PrEP uptake and adherence. One of our next steps will to be to include trans women who inject drugs as well.”
In the study, the authors described how women who inject drugs are more likely to share syringes than men, leading to greater risk of HIV exposure. “In part, [women’s risks are] shaped by having to negotiate prevention methods (e.g., condoms or new syringes) with male partners, which has been shown to impede their use.”
The researchers required the women to receive the medicine through their own health insurance, but were able to assist those who didn’t already have insurance in getting it.
Cost and insurance barriers keep many at-risk people from accessing PrEP. Fewer than 10 percent of people who would benefit from PrEP medication can actually get it. Out-of-pocket costs for the drug and lab tests can surpass $1,000 a year. Despite the Affordable Care Act now requiring most private insurers to cover the drug, technical loopholes abound even for those with insurance.
An Underused Resource
The women who took agreed to take Truvada were disproportionately likely to be those who accessed an SSP often, who didn’t necessarily always use condoms and who had experienced sexual assault. Most reported engaging in sex work.
Forty-two women, or nearly 45 percent of participants, took the Truvada through all 24 weeks. However, many did not take the medication every day as recommended, which can render it less effective. Overall, the women reported being satisfied with the medication and not experiencing any significant side effects.
“Integrating PrEP with SSP services is feasible and acceptable for women who inject drugs,” the authors wrote. “This supports that daily PrEP is a viable prevention tool for this vulnerable population.”
How can we interpret this research? For starters, we have to consider why administering PrEP through an SSP was effective. Often, SSP provide much more than just syringes. They distribute first aid supplies, personal protective equipment, naloxone, clothing and even food. They often provide safe physical spaces for people who use drugs—like a private bathroom where it’s understood they may inject, or a communal room with a television, furniture, computers, phones and hot coffee.
Many of them also provide referrals to medications for opioid use disorders (MOUD), social counseling, support groups and even safe consumption sites (SCS) in countries that allow them. By having all these necessities under one roof, as well as humanizing face-to-face interactions with friendly local harm reductionists, SSP develop goodwill and trust with the communities they serve.
That’s why co-locating HIV prevention medicine and SSP in the same building can help people achieve better health outcomes. Just ask the staff at the Humboldt Area Harm Reduction Center in northern California: Despite more than 90 percent of drug user connected to MOUD staying in treatment, they were thanked by being driven out of their home city of Eureka.
PrEP cut the risk of HIV infection by half, and also resulted in fewer instances of syringe-sharing.
Previous research has also shown the effectiveness of giving PrEP to people who inject drugs. A landmark clinical trial in Thailand that ran between 2005-2012 studied a group of over 2,400 HIV negative men aged 20-60 who injected drugs. PrEP cut the risk of HIV infection by half, and also resulted in fewer instances of syringe-sharing. The participants were also offered “risk-reduction” counseling and opioid substitution therapy, but were not required to engage in either.
“Nearly one in five people nationally who screen positive for HIV are women, the majority of whom are women of color, especially Black and Latinx women,” Roth said. “It’s clear that tailored programming is needed to address their specific HIV prevention needs. Women have been under-represented in all phases of PrEP research. Key is remembering that one size does not fit all, and just because we build it doesn’t mean they’ll come.”
Photograph via Wikimedia Commons/Creative Commons 2.0