In March 2020, to reduce the risk of COVID-19 infections among patients and staff, the Substance Abuse and Mental Health Services Administration (SAMHSA) and the Drug Enforcement Administration (DEA) made an unprecedented decision that made it a whole lot easier to get take-home doses of methadone. They issued temporary guidelines allowing clinics to dispense 28 days of take-home doses to “stable” patients and 14 for less “stable” patients. Normally, to methadone patients’ chagrin, it can take years to “earn” this many take-homes.
Last month, a second historic decision was announced: SAMHSA is “extending the methadone take-home flexibilities for one year, effective upon the eventual expiration of the COVID-19 Public Health Emergency … SAMHSA is also considering mechanisms to make this flexibility permanent.”
A SAMHSA representative told Filter that the decision was made by “consulting with the DEA, state partners and many treatment stakeholders.”
“It shouldn’t take a global pandemic for them to listen to us.”
For over 30 years, methadone clinics have been impervious to change, it’s as if they exist in a snow globe. COVID-19 acted like a force multiplier and opened clinic operating procedures up to scrutiny.
“It shouldn’t take a global pandemic to get more take-home doses,” Louise Vincent, the executive director of Urban Survivors Union (USU) and a methadone patient, told me in an interview for a documentary I’m making about methadone and COVID-19. “It shouldn’t take a global pandemic for them to listen to us.”
But that is exactly what it took. Clinics are superspreader sites as a result of their rigid structure. Hundreds of people travel to them six days a week, many by public transportation. They often stand in long lines, wait in small crowded rooms to be observed ingesting medication, and sit in mandatory group counseling sessions where social distancing is impossible.
Methadone clinics had no choice: Allowing more take-homes was the only way to reduce the spread of the coronavirus among a medically vulnerable population. And for some it was liberating. One patient explained, “I am able to live a normal life without having to come in every single day. I have a baby at home … I feel a little more independent. I feel when I do get a job it will be a lot easier …I just enjoy being able to be more like a normal person, just having my medication at home.”
But the reality is that the new policy was adopted inconsistently across the country. As Filter has reported, many clinics didn’t provide any 14- or 28-day take-home doses. In interviews with patients around the country, several told me they had never even heard about the revised take-home dose policy.
That’s because the SAMHSA guidelines are voluntary, and the decision to implement them ultimately rests with state authorities—like the Office of Addiction Services and Supports (OASAS) in New York—and with the medical directors of opioid treatment programs (OTPs), as methadone clinics are also known.
“Until we are out of this culture of cruelty that exists in the clinic system, we are still in a place where people are being hurt.”
“While I applaud SAMHSA’s decision to allow the covid take-home flexibilities to remain for a year, it is a small incremental step when we need drastic widespread change,” Nick Voyles, a hepatitis C liaison at USU, told Filter. “Unfortunately, until we are out of this culture of cruelty that exists in the clinic system, we are still in a place where people are being hurt. Too much depends on the clinic being in charge.”
In what can only be considered a regressive move, some clinics that offered more take-home doses began decreasing them once the pandemic had somewhat receded and vaccinations were available. A patient on methadone in Boston, who has diabetes, said that his clinic stopped giving him 14-day take-homes without providing an explanation. He’s back to six days a week now, and is so angry he’s trying to transfer to a clinic that still provides that number of take-home doses.
Almost two years after the policy was first enacted, a number of studies on the effects of relaxing the take-home doses policy show that doing so did not increase fatal overdoses or “negative treatment outcomes,” and “diversion” was rare.
The scaremongering that we’ve heard ad nauseam from the drug warriors at the DEA—which, inexplicably, oversees methadone clinics—has always claimed that if people had access to more doses of methadone, they would either sell it (diversion) or die (overdose.) It was never true, but now there is empirical evidence to prove that better methadone access does not cause harm.
“Our research highlights the need to consider permanently loosening the restrictions on methadone take-home doses,” said Ofer Amram, an assistant professor at Washington State University, “which would help many people who are struggling to access opioid treatment.”
Another call for reform has come from the American Society of Addiction Medicine (ASAM), a professional medical society representing over 6,500 physicians, clinicians and associated professionals. Normally cautious and conservative, ASAM published a public policy statement with a series of progressive recommendations for pharmacy dispensing, methadone vans, telemedicine evaluation for methadone and not demanding counseling as a condition to get medication, among many others.
What took SAMHSA so damn long?
Finally, SAMHSA is recognizing that reforms are needed. A November press release stated, “The flexibility promotes individualized, recovery-oriented care by allowing greater access for people who reside farther away from an OTP location or who lack reliable transportation. Fewer visits also means people generally have more time to work, care for loved ones, and conduct other routine activities in their daily life.”
But what took SAMHSA so damn long? How did the abysmal retention rates in OTPs—which they are fully aware of because they study them—not tip them off that something was fundamentally wrong? Why—during the ongoing opioid-involved overdose crisis, which has tragically killed nearly 841,000 people since 1999—didn’t they use their power to eliminate the numerous, well-documented barriers to getting and staying on methadone which is proven to cut the overdose death rate by 50 percent or more?
For that epic failure, SAMHSA and the DEA, who are responsible for regulating OTPs at the federal level, have blood on their hands. How many people would be alive today if they had made it easier to get a 28-day supply of methadone than to inject fentanyl? Can it really be only now, as a result of the pandemic, that SAMHSA suddenly realizes traveling long distances six days a week to swallow a single dose of methadone is a massive, time-consuming, costly hardship and that fewer visits to the clinic allow patients to get on with their lives and feel “normal”?
SAMHSA has worked hand in hand with the DEA, an international police organization dedicated to fighting the War on Drugs, to block clinic reform for decades. Methadone patients have paid with their lives for the intransigence of these federal agencies.
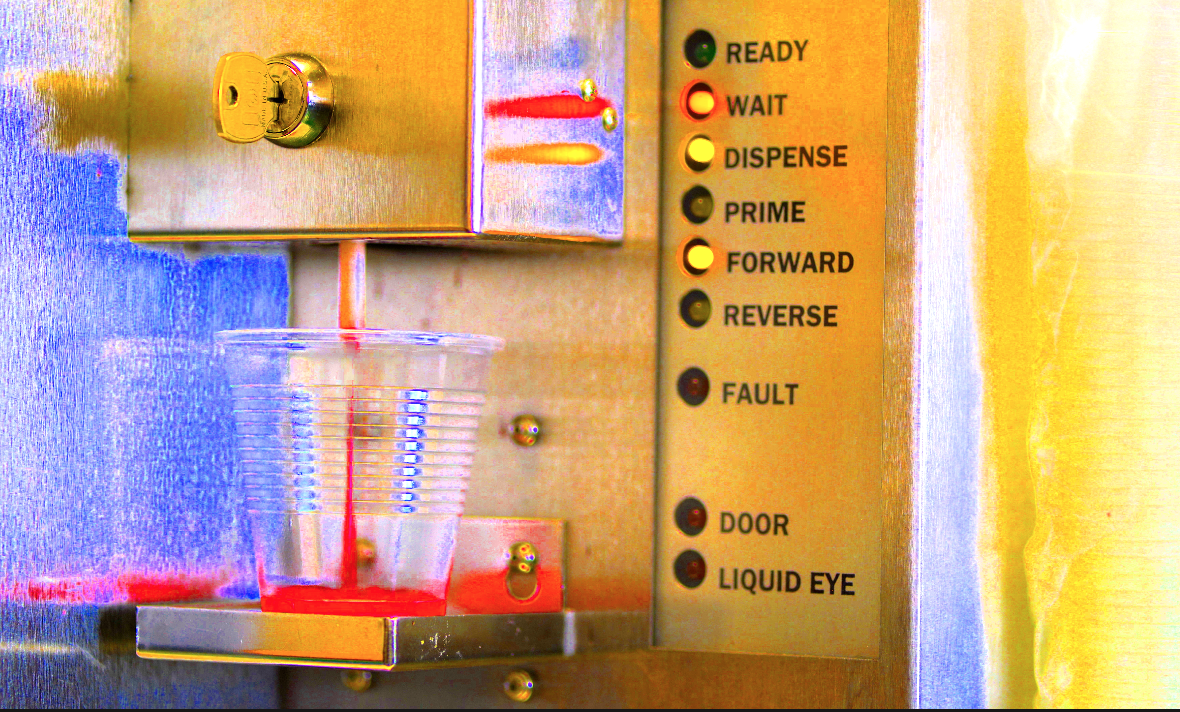
Photograph by Helen Redmond and Marilena Marchetti




Show Comments