You might have seen the recent article about an 18-year-old who vaped for two years and was told by a doctor that he now has the lungs “of a 70-year-old lifetime heavy smoker.”
What caused this and other vaping-related cases of lung damage became clearer in the past week, when the FDA announced that the majority of such cases were due to adulterants in illicit “products containing THC.” The conflation of these illicit THC vape products with nicotine-containing products has likely left many people confused.
Is it still true that vaping nicotine is substantially less harmful to health than smoking (but not risk-free), as reported, for example, by the National Institute for Health and Care Excellence in the United Kingdom? Or, do we follow the new warnings from the California Department of Public Health to stop vaping completely?
Perhaps the answer can come from an unlikely hero: that 70-year old lifetime heavy smoker we were talking about.
What kind of facts do we have about that person? And what do they tell us about the potential for nicotine vaping to reduce the harms of smoking?
The first fact is the harshest. Most smokers don’t make it to 70 because they die an average of 10 years earlier than non-smokers.
They include my dad, who died a daily smoker at age 63. I wrote his obituary five years ago today. In that same year (and each year before and after), well over 400,000 other obituaries could have been written describing lives that ended early due to smoking-related disease. The number of smokers who die prematurely could fill seven pro-football stadiums every year.
Over time, Bob’s side-stream smoke and chattiness grew on me. We were a fit from the start.
But with advances in science and healthcare, a good number of smokers are living well into their 70s despite the damage done by cigarettes. One of those older smokers happened to be my neighbor. I’ll call him “Bob.”
Bob had a gray, wispy mustache and liked to smoke cigarettes on his front stoop looking out over the narrow, cracked alley we shared on the east side of Baltimore. It was 2008 and I had just moved to town, with student loan debt and a recession rolling in. Over time, Bob’s side-stream smoke and chattiness grew on me. We were a fit from the start—I was in need of friends and conversation, and he had an affinity for both.
I learned he had grown up in a blue-collar suburb not far away, and had recently let go of his cross-country trucking route for a local gig. He wanted to slow down and buy a motorcycle he could ride through the tree-lined backroads of Maryland. He was in his 70s and lived with his older brother in a tiny rowhouse his family had owned for decades. His brother had severe emphysema (I’m guessing from his own years of smoking) and mostly stayed inside with his oxygen tank while Bob held court on his front steps.
After a few weeks of small talk, Bob asked what I did for a living. I told him I was a scientist up the road at Hopkins, starting a fellowship in addiction. In fact, I said, gesturing towards the cigarette burning between his fingers, I spent nearly six years in graduate school studying smoking.
That caught his attention. He wanted to know what I knew—were cigarettes really that bad for people? He had started smoking in high school, and once he joined the military the habit stuck. He had tried to quit, but nothing helped. The patch and gum were useless.
I can’t remember exactly how I responded, but I know I paused. Who am I to tell a 70-year-old what to do with his body or health? For all I knew, cigarettes were one of the most enjoyable parts of his day. And how was I going to tell him something new about cigarettes when he had smoked over 300,000 in the last 50 years? He was more of the cigarette expert than me.
I’ve since discovered that older smokers, like all of us, have a lot to learn about smoking. Older people are more likely than younger smokers to think that the evidence about the harms of smoking has been exaggerated, and that smoking is something they can do little to change. They are also more likely to inaccurately believe that nicotine is the primary disease-causing ingredient in cigarettes, and that cigarettes without nicotine are safer than those with nicotine.
Quitting can add years to your life regardless of your age—including people 80 years and older.
Perhaps all this misinformation has kept some of these older smokers, well, smokers. A recent US-based survey found that nearly a quarter (24.2 percent) of smokers aged 65 and over reported never planning to quit smoking—compared to only 9.8 percent of 18-to-34-year-old smokers. And a separate report from the CDC found that smoking cessation rates are significantly lower for older compared to younger smokers.
But all hope is not lost if a person finds themself aging into smoking. Quitting smoking can add years to your life regardless of your age—including people 80 years and older. And if complete cessation isn’t possible (as was the case for Bob), then evidence suggests that reducing the number of cigarettes smoked per day can also benefit older smokers.
Yet I decided to not say much to Bob about cigarettes. I didn’t want to be preachy, I just wanted to be someone he could count on. Like some sort of weird friendship sitcom about a 30-something lady with a cat and her 70-something gruff neighbor with a smoker’s cough.
But Bob was definitely the better friend. In the winter he cleared the snow and ice on my steps (hours before I woke up), and was always sure to add a coat of salt so I didn’t slip as I walked to my car. And in the summer, he would bring me fresh fish that he caught during his weekend trips to the Chesapeake Bay, wrapped delicately in parchment paper.
He yelled at the construction crew working on the townhouse next to me when he caught them stealing electricity from my outdoor plug. And when he finally got that motorcycle, he waited next to it until I stepped outside, so he could show off its extra seat he got installed in case I ever wanted to take a ride.
And one time, he brought me roses.
It was early December 2012, and I was going through a couple of back-to-back break-ups. Unexpectedly, on a crisp, gray afternoon, I heard a knock on the door and opened it to see Bob handing me a vase overflowing with flowers.
He waited on my steps as I read the small card sandwiched between the petals and stems: “I hope these flowers will mend the broken heart that those two guys gave you. I always be here for you.”

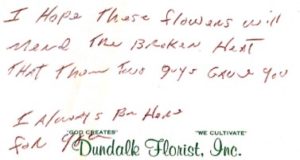
Cards from “Bob,” with identifying details redacted.
Soon after I found Bob on my front stoop with those roses, he was diagnosed with lung cancer.
The treatment would include surgery and chemotherapy, and he was scared. His treatment moved fast, and I watched as his body and energy withered with each update he gave me on his weekly outpatient appointments. He had to sell his motorcycle to pay for the costs of his healthcare. He lost one of his lungs in surgery.
When I saw him outside smoking one afternoon, I couldn’t resist asking: Had he thought about switching to e-cigarettes instead?
I explained that they were new to the market but didn’t burn, so wouldn’t deliver the carbon monoxide he inhaled when smoking. This was around 2014 so we had yet to learn what leading scientists now say—that we could save at least 1.6 million early deaths, if all smokers in the US switched to vaping over the next 10 years. This is because completely switching significantly reduces exposure to known toxicants found in combustible cigarettes.
His doc said that e-cigarettes hadn’t been studied long enough, weren’t recommended by the FDA, and weren’t worth the risk. So Bob kept smoking.
It turns out Bob did know about e-cigarettes, even if he didn’t know these facts, and had asked his surgeon about them. But his doc said that e-cigarettes hadn’t been studied long enough, weren’t recommended by the FDA, and weren’t worth the risk. So Bob kept smoking.
When Bob moved away, he told me I could visit him at his new assisted living home. His brother had passed away and he didn’t have the money to keep paying rent to his family. When he let them know, they decided to sell it. And although his cancer was in remission, he needed help getting around because his breathing was getting worse. He coughed all the time.
I moved soon after, and just like the motorcycle ride I had passed up a couple years before, I never took him up on that offer for a visit. Maybe I’m sharing his story to make amends.
Bob’s story, and the millions of others like it, should be a call to action to shift the debate around the risks and benefits of vaping to include all ages of nonsmokers and smokers. The debate is false and incomplete if we continue to focus on youth and young adults to the exclusion of older smokers—the population that carries the greatest burden of smoking’s harms.
Aging smokers deserve more than a brief mention in a catchy article offering sensationalized news on youth vaping. They deserve to be the headline about the potential for cigarettes to be made obsolete by technological innovation, such as vaping products that can serve as safer, effective and appealing substitutes for smoking.
Every day, 1,300 Americans lose their lives to smoking-related illness and most of them are older adults. Each of these lives has a story—a story cut short because we have yet to use our scientific and regulatory resources to make harm reduction products and information fully available to the smokers who have not been able to successfully quit.
The lives of our oldest smokers are worth just as much as those of our youngest.
This article is dedicated to the author’s father, Dr. Ray Kleykamp (1951-2014).
Top photo by Patrick Hendry on Unsplash




