On January 7, an association of Massachusetts health professionals released a resource to guide hospitals in the state (and elsewhere) in implementing lifesaving treatment for opioid use disorder in their emergency departments.
Governor Charlie Baker signed a law last August that required medication-assisted treatment (MAT) for opioid use disorders to be offered in emergency departments (ED) in the state. But the law will only be effective if MAT is widely implemented and accessible.
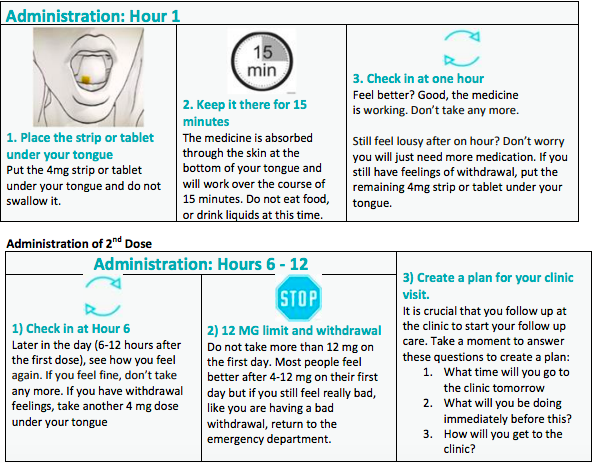
That’s why the Massachusetts Health & Hospital Association (MHA) has released the new roadmap. It includes: recommendations that hospitals employ “Recovery Coaches (RC) and Recovery Support Navigators (RSN);” examples of criteria that qualify patients for MAT; and fact sheets on buprenorphine use for doctors to give to patients (below).
The guidelines also reveal how much misinformation, discrimination and simple bad judgment is out there when it comes to addiction, even in the medical field. For example, the authors felt the need to tell medical professionals not to engage in “extended interviews or discussions about treatment options” while a patient is actively going through withdrawal. “Patients in acute withdrawal may be extremely uncomfortable and find it difficult to engage,” the authors write.
And, as if mitigating patient pain isn’t enough of a motivator for doctors, the guidelines state: “These patients are also at high risk of leaving against medical advice to use opioids from another source if their withdrawal is not adequately treated.”
But the consequence isn’t simply that patients will “use opioids from another source,” according to Leo Beletsky, a professor of law and health sciences at Northeastern University. It’s the difference between life and death.
“When revived and transported to the hospital after an overdose event, people who use opioids will experience rapid withdrawal. If medications are not provided to address their symptoms and cravings, many will leave against medical advice. This puts them at an extremely high risk of fatal overdose,” Beletsky tells Filter.
Because of this, emergency departments are critical sites for harm reduction intervention for “patients who have experienced health complications related to opioid use, including abscesses, overdose as well as a wide variety of other general health conditions,” says Dr. Kimberly Sue, medical director of Harm Reduction Coalition. “These guidelines provide important clarity and frameworks for initiating medication for opioid use disorder in the EDs.”
Similarly, emergency services are important for addressing opioid overdoses because they have become “the main source of health care for many of our society’s most vulnerable,” Beletsky says, adding that “making MAT available in these settings is an important way to connect people with the care they need when they need it.”
The guidelines also note the concern that doctors will feel “uncomfortable” giving patients buprenorphine to take home “due to threat of poisoning if children get hold of it.”
“This is an important fear,” the authors write, “but we discharge patients home with lots of medications that would pose a safety risk if a child ingested them. While this is understandable in light of a recent study/publicity, in fact buprenorphine is usually dispensed in childproof envelopes, and it is no more risky to children than the more common practice of dispensing 20 mg of oxycodone, for example. The risk is greater to children at home if the parent continues to use heroin/fentanyl than if s/he is discharged with buprenorphine.”
Ali Raja, chair of the MHA workgroup on MAT and executive vice chair of Massachusetts General Hospital’s Department of Emergency Medicine, sees the guidelines as the next step for the state’s response to the overdose crisis. He says the guidelines are “designed to give the clinicians the tools they need to accomplish the ultimate goal of supporting patients as quickly as possible and help them get their lives back.”
Photograph: TopsImages