On September 22, the Food and Drug Administration announced that harm reduction naloxone suppliers are exempt from wholesale pharmaceutical distribution restrictions, effective immediately. This de facto waives naloxone’s prescription requirement at the federal level, allowing the broader harm reduction community to purchase and distribute naloxone in bulk for the first time.
There is no precedent for the FDA’s new guidance; the agency has never publicly backed harm reduction policy with this much specificity. Remedy Alliance was the first to identify the mechanism that supports the guidance—an exemption within the pending Drug Supply Chain Security Act (DSCSA) that removes the traditional distribution barriers for drugs relevant to current public health emergencies.
Since April 1, Remedy Alliance has been asking the FDA to declare that harm reduction groups distributing naloxone qualify for the exemption, as well as instruct states to abide by it immediately rather than wait until the DSCSA becomes law in 2023.
Working under that same urgency, Remedy Alliance—known for the past decade as the Opioid Safety and Naloxone Network Buyers Club—launched its in-house affordable naloxone distribution on August 1. The first shipments from Pfizer and Hikma were arriving at its warehouse after a 13-month shortage that exhausted the harm reduction community’s resources and caused, by Remedy Alliance Board President Dr. Nabarun Dasgupta’s estimation, 12,000 to 18,000 excess deaths.
It would have been ideal to have FDA backing at the time of the launch, but the only choice was to move forward.
🚨 Something huge happened today. 🚨@US_FDA @DrCaliff_FDA listened to harm reduction programs and made it infinitely easier to purchase #naloxone in bulk. With 100,000+ overdose deaths each year, we need BIG solutions.
w/@RemedyAlliance @ejwheeler9 @coreysdavis
🧵 1/26 pic.twitter.com/HifngvMOMu— Dr. Nabarun Dasgupta (@nabarund) September 23, 2022
Naloxone is still a prescription drug. But this guidance circumvents, in one fell swoop, the entire bureaucratic patchwork of state-level regulations that have long prevented most harm reduction groups from wholesale distribution. The high-threshold requirements included having a unique DEA-licensed prescriber and commercial shipping address, and administrative barriers so cumbersome most groups couldn’t even accept naloxone that manufacturers tried to give them for free.
“If we were required to operate within pharmaceutical wholesale distributor regulations, we would be required to reproduce the barriers that programs already experience,” Remedy Alliance Codirector Maya Doe-Simkins told Filter.
“So if we want to knock out the barriers, we can’t be a wholesale distributor. We can’t operate in that way. Similarly, we can’t operate as a specialty pharmacy, or a closed-door pharmacy; those regulations that rule those entities require the replication of those barriers.”
Though the guidance doesn’t reference anyone by name, it does endorse the very specific model Remedy Alliance has been operating in a slight gray area since August. It also clearly communicates that there’s interest within the FDA, and by extension other federal agencies, in removing naloxone access barriers for harm reduction—not just because it says that, but because it left the definition of “harm reduction suppliers” helpfully broad.
The term can certainly be applied to the small number of other groups doing their own form of mutual aid distribution, including NEXT Distro, Smoke Works and Points of Distribution. It could also apply to larger syringe service programs (SSP) well-positioned to function as distribution hubs to smaller groups in their communities. The ability to easily accept and distribute donated naloxone is particularly significant for Direct Relief, which receives large volumes of donated naloxone through a partnership with Pfizer.
Remedy Alliance is so low-barrier that there will almost certainly be programs that want to switch over from their state procurement system, even though that Narcan is free.
State boards of pharmacy have to adhere to the DSCSA, so this exemption opens up a new channel in states where naloxone has been least publicly accessible. Traditionally, the twin gatekeepers were prescribers and pharmacists; this bypasses both.
“We can use this mechanism for advocacy purposes,” Doe-Simkins said. “To relay to other entities the FDA does not have control over how [the federal government is] emphatically in support of expanded access.”
In response to Filter’s request for comment, the FDA indicated that the Overdose Prevention Framework, introduced August 30, was the catalyst for the exemption. Despite a media characterization as harm reduction-forward, the Biden Administration has not stepped outside traditional drug policy since cowing to racist backlash in February around ambiguous language in its marquee federal grant that might have finally allowed sanctioned SSP to purchase crack pipes with their federal funding. Naloxone access is broadly popular was never likely to face that level of pushback, but for the FDA to come out with such an unequivocal show of support bodes well for federal harm reduction policy.
In the long battle for naloxone liberation, the FDA guidance represents harm reduction’s third major innovation: interpreting state-wide standing orders for harm reduction purposes, a template that began with Massachusetts in 2007 and has since been enacted by all 50 states, DC and Puerto Rico; negotiating the historic 2012 deal that made naloxone affordable and accessible through what was then the Buyers Club and today is Remedy Alliance; and now authorizing harm reduction groups buying naloxone in bulk to bypass wholesale distribution restrictions. All that’s left is to take down the prescription status itself.
YES! been advocating for OTC for decades! @RemedyAlliance & affiliates are on track to move more nlx than every single pharmacy in the country combined. Pharmacies got some work to do to be welcoming to PWUD! HR orgs need more 🙏❤️💲💲💲
— Remedy Alliance/For the People (@RemedyAlliance) September 23, 2022
“This is intentionally meant to be a free-market deregulation kind of guidance,” Dasgupta told Filter. “Naloxone has been effectively a monopoly, with a couple of generic manufacturers, and the purchasing power of harm reduction programs has been sidelined by the high costs. And the corporate focus on the nasal spray.”
The thing about the distribution model pioneered by Remedy Alliance is that it’s so low-barrier there will almost certainly be programs that currently get Narcan through their state procurement system, but want to switch to generic naloxone from harm reduction suppliers instead, even though the state systems are free. The inordinate administrative burdens that go along with government-funded Narcan are a strain for pretty much everyone, especially in the most overregulated states like Ohio.
The FDA exemption could potentially mean a shift in momentum away from the overpriced nasal sprays and toward unbranded injectable naloxone—which has been the more effective, more cost-efficient and more humane product all along.
“Not totally sure,” Doe-Simkins said. “But trust and believe that we’re going to work on that.”
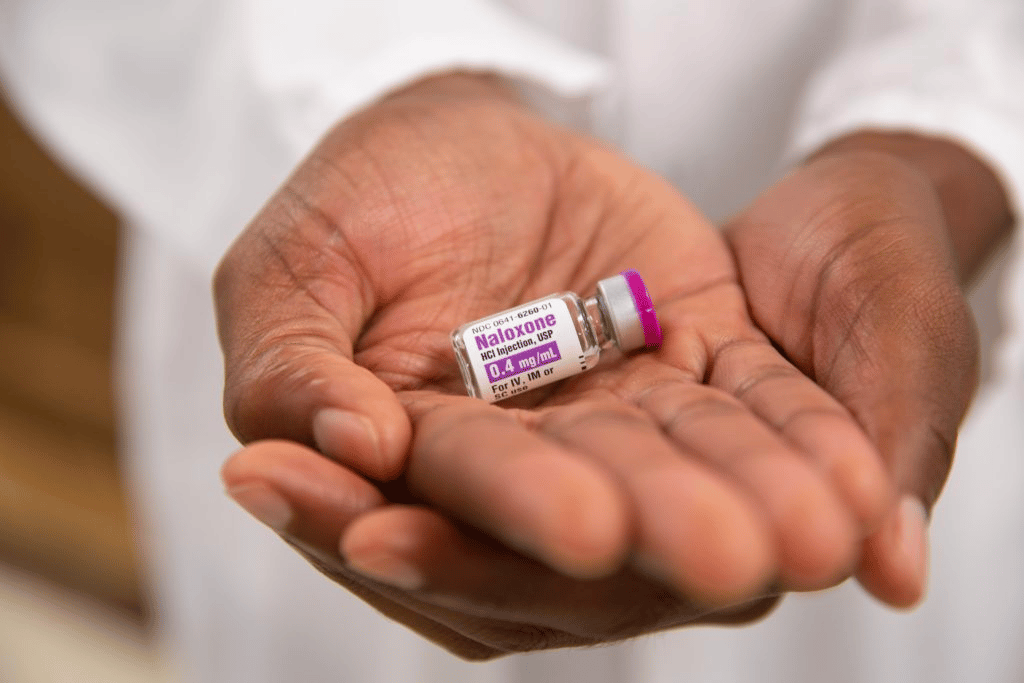
Photograph courtesy of Bridget Horgan Bell
Read Filter‘s previous coverage of Remedy Alliance’s naloxone distribution here and here