In the wake of the unprecedented outbreak of HIV among people who inject drugs in Scott County, Indiana 4 years ago, public health officials, politicians and researchers have spent a great deal of time seeking out the causes of the outbreak and identifying ways in which it could have been prevented.
According to a soon-to-be-released study* from the Brown University School of Public Health, the answer is a relatively simple one: Set up syringe services programs (SSPs) and set them up early.
At the 2019 International Harm Reduction conference in Porto, researcher William Goedel presented the findings from a mathematical modeling study that aimed to simulate what the average rate of HIV transmission would be in Scott County under the three separate scenarios.
In the first scenario, Goedel and his colleagues measured HIV transmission rates when an SSP is established in the community before a non-virally suppressed person living with HIV entered the drug using community.
In the second scenario, the study examined what HIV transmission rates would have been had an SSP been set up after 10 people who use drugs had contracted HIV.
And in the third scenario, the researchers modeled what the average rate of HIV transmission would be if there was no SSP at all.
Unsurprisingly, Goedel’s modelling found that SSPs were very effective in reducing transmission of HIV among people who inject drugs, and that establishing an SSP before the initial HIV transmission better prevents the spread of the virus than when the SSP is set up early on in the cycle of the outbreak.
After running 1,000 simulations in each of the three scenarios, the study estimated that an average of 133 people in Scott County would contract HIV over a five-year period if no SSP were present (the real-life outbreak in 2014-15 resulted in 215 people contracting the virus).
However, if an SSP were introduced proactively into Scott County before any HIV transmissions had taken place, the simulation showed only an average of 27 cases of HIV transmission over five years, representing a reduction in HIV incidence of nearly 80 percent.
Under the scenario where an SSP was introduced reactively, after 10 individuals had contracted HIV, there were still considerable reductions in new cases of HIV, with an average of 57 people contracting the virus over five years.
It is always useful when harm reduction advocates are provided with additional peer-reviewed studies that reinforce the utility of SSPs.
The results of this study are not surprising, as there is already a long evidence base that shows SSPs significantly curb HIV transmission among people who inject drugs—and a previous modelling study on whether or not an earlier response in Scott County would have effected the dynamics of the HIV outbreak by researcher Gregg Gonsalves, published in the Lancet last year, had similar results.
All the same, it is always useful when harm reduction advocates are provided with additional peer-reviewed studies that reinforce the utility of SSPs when speaking with government officials who erroneously view syringe access with suspicion.
It is worth noting that the results of this study are specific to Scott County, Indiana and may not reflect the impact of SSPs on other communities. That said, the effectiveness of proactive SSP initiation in this study—combined with the mountains of evidence showing the positive impact of SSPs in reducing HIV transmission among people who inject drugs—leaves little doubt as to the need for SSPs to be a part of the US response to the opioid-involved overdose crisis.
*The full study, entitled “Implementation of syringe services programs to prevent rapid HIV transmission in rural counties in the United States: A modeling study,” is set to be published in an upcoming issue of the journal Clinical Infectious Diseases.
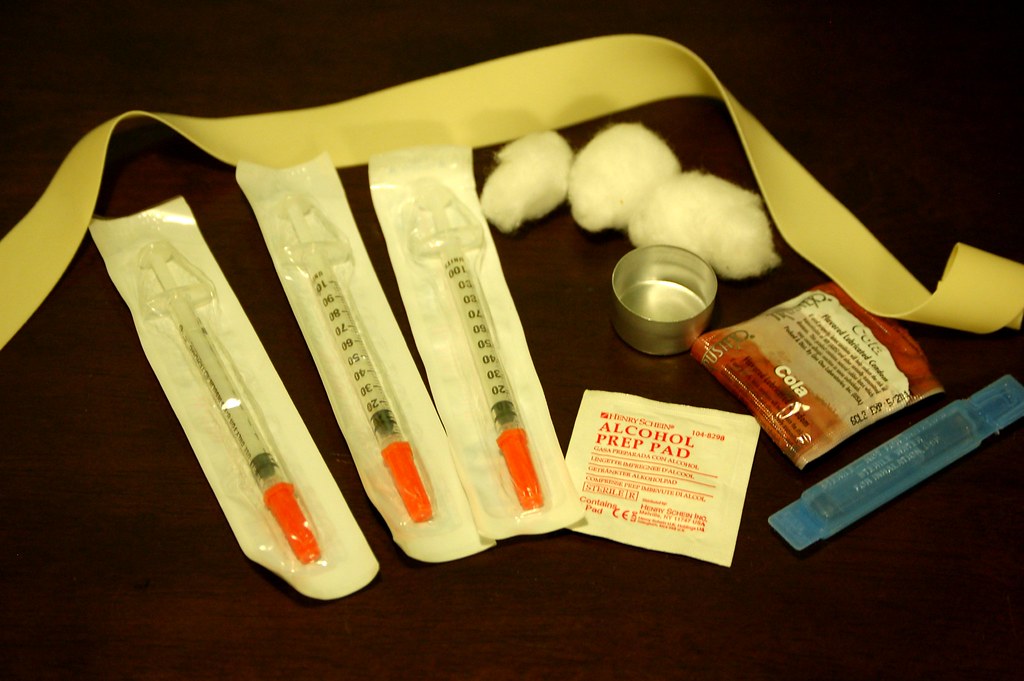
Photo via Todd Huffman / Creative Commons




Show Comments