The monkeypox epidemic isn’t going anywhere, especially for street-based sex workers. NPR reports that cases of infection have slowed down in some metropolitan areas, including New York City, San Francisco and Chicago. However, public health experts temper optimism with caution, when vulnerable populations remain at risk for contracting the virus.
Monkeypox (MPX) is transmitted through close skin-to-skin contact and anyone, regardless of their identity, can contract the virus. While it’s not a sexually transmitted infection, skin-to-skin during sexual intimacy means that people engaged in street-based sex work are particurly at risk.
Solana Sparks, a full-service sex worker based both in Seattle, Washington and San Juan, Puetro Rico, acknowledged that while cases are fairly low in Washington state, she tours outside of the area and the United States for her job. At the time of the interview, she was planning to travel to New York City, which had 3,339 active MPX cases as of September 9 per city data.
“A lot of us are just really scared and trying to do our best to take care of ourselves.”
“Many of us are not only concerned about our health and not wanting to be what a lot of people see us as—vectors of disease—many of us [financially] support whole family systems and friends,” Sparks told Filter. “If we are to get sick and can’t work for a month, or over a month, we would destabilize our whole ecosystem, [and] ourselves. Also, if we have scars and things, we’re really screwed. A lot of us are just really scared and trying to do our best to take care of ourselves, our communities, and our clients.”
She added, however, that New York’s sex worker-inclusive vaccine rollout made her feel “more relaxed” about her planned travel. “I am pleased to see one of the cities with the highest rates expand access to additional high risk populations,” she said. “I hope other cities will see this response … and include sex workers in priority vaccination population categories before a breakout. I just got vaxxed so have to wait, but am excited to know that I can get access in NYC in a way that has been difficult in Seattle.”
While vaccines have been successfully rolled out in major cities, not everyone has the same access because eligibility criteria vary by jurisdiction. Initially, many health departments reserve eligibily for those who’ve been exposed and/or fall under the designation of “MSM,” an abbreviation for men who have sex with other men.
Fourtunately, for Sparks and other sex workers, New York City has more expansive eligibility criteria; additionally, second doses are now available to those who’ve received the first dose at least 10 weeks previously. However, vaccine access still isn’t equal, as racial disparities show.
Despite the misconception that sex workers are overwhelmingly women, there are many sex workers of varying gender and sexual identities with clientele of varying indentities. Many within this community face stigma, discrimination, and overall lack of access to quality health services, even those as obviously critical as STI testing. Of course, men who have sex with other men can be sex workers. But many sex workers who don’t identify as MSM are still at great risk, particularly when we know that men who have sex with men also have sex with other genders.
Pittsburgh-based full-service sex worker and writer Jessie Sage attempted to receive an MPX vaccine in late July. Just like wearing condoms, taking PrEP (pre-exposure prophylaxis) and getting regularly STI tested, she sees the vaccine as a protective harm reduction measure for her health, accepting she can’t guarantee to know the status of her clients. However, she was turned away because the state of Pennsylvania only scheduled appointments for men who have sex with other men, along with transgender, nonbinary and gender nonconforming people.
“I feel I shouldn’t have had to explain why I needed [the vaccine] and I shouldn’t have to out myself in order to get it.”
“All of the health care providers were very aware that it makes sense to give [the vaccine] to sex workers and they really wanted to help us, but felt hands tied behind their back,” Sage told Filter. “I didn’t feel like they were blowing me off.”
Days after she published a piece about the incident, though, she was finally able to receive a vaccine. She was scheduled for her second during the first week of September.
“Us—massage therapists, daycare workers, anyone who has close physical contact with other people, including naked physical contact with other people—should be prioritized,” she said. “I feel I shouldn’t have had to explain why I needed [the vaccine] and I shouldn’t have to out myself in order to get it. We should be able to self-identify [as high risk] without having to disclose. What I think should’ve happened from the beginning is that [health agencies] should have taken anyone who feels like they are at high risk for this seriously and given the vaccine to [those] who opted into it.”
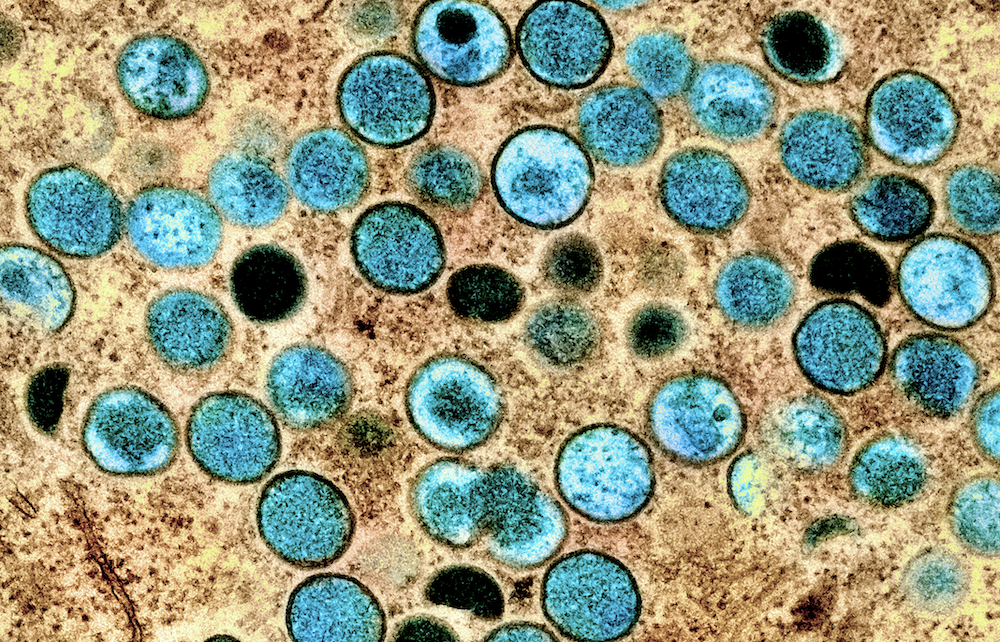
Image of colorized transmission electron micrograph of monkeypox particles (teal) found within an infected cell (brown), cultured in the laboratory, by the National Institute of Allergy and Infectious Diseases via Wikimedia Commons/Creative Commons 2.0




Show Comments