A few weeks back, Soma Snakeoil, an artist and the founder of Los Angeles-based organization the Sidewalk Project, came across a man overdosing on a street corner. She asked his girlfriend what he had taken and administered naloxone, but he was still non-responsive.
Working quickly, she created a cone with her hands, and performed rescue breathing on the man. He came to, and an ambulance, called by her friend, showed up and took over.
“I was not thinking about the pandemic. I ripped off my mask and it was on,” Snakeoil said.
Since the start of the pandemic, harm reduction organizations like the Sidewalk Project have been forced to change the way they provide care and support—others have closed entirely. While many remaining operations are still handing out naloxone and syringes and reversing overdoses, the work has grown harder and, in light of COVID-19, more perilous. In the United States and Canada the pandemic has also led to a sharp increase in the number of overdose deaths.
Administering naloxone, issuing rescue breath and supervising injections, are all close-contact work, which can be risky at the moment, according to Jade Boyd, a professor in the department of medicine at the University of British Columbia. “There is an increased risk of infection for diseases like COVID when you’re working in a high-contact space,” she said.
Boyd is one of the authors of a recent commentary published in the International Journal of Drug Policy, which outlines how some of the pandemic-related vulnerabilities for frontline harm reduction workers disproportionately affect those in “peer” roles—positions defined by a person’s lived experience, including past or present drug use.
While the challenges of working in harm reduction during a pandemic are taxing to staff across these organizations, people in peer roles can have it particularly bad. Many work in temporary, volunteer, on-call, part-time or other tenuous roles. And although work schedules that aren’t strictly nine-to-five can be helpful for people who use drugs, these positions come with a slew of disadvantages, Boyd said.
There is usually a pay discrepancy between peer and non-peer positions. Additionally, peer workers are less likely to get health benefits or paid sick leave—particularly big issues during a pandemic—as well as access to unemployment insurance or vacation time to ease the emotional toll of the high-stress work.
“All these issues become really heightened during the dual pandemics,” Boyd told Filter.
While the paper is based in a Canadian context, parts or all of it may be applicable internationally, she added. However, types of harm reduction organizations vary from place to place, as do the needs of each community.
“When somebody ODs, we’re the ones bringing them back. I would like to see that we’re recognized for the work.”
Lorna Bird is a peer worker with the Vancouver Area Network of Drug Users (VANDU), and a former board member and supervisor for the organization’s overdose prevention room. She has seen firsthand the impact that Canada’s drug war has had on some communities, and that experience informs her work.
But in many cases, the peers work long hours every day; they make CA$12 an hour if they work the injection room, or $10 an hour if they work reception. Similarly, she said, peer workers don’t get paid vacation or other benefits.
Bird doesn’t think the pay discrepancy is fair. But perhaps more than that, it bothers her that her colleagues are not called frontline workers even as they work on the front lines, administering naloxone and providing other forms of care.
“When somebody ODs, we’re the ones bringing them back,” Bird said. “I would like to see that we’re recognized for the work that we do.”
Snakeoil—who has lived experience, but is not a “peer” worker in that sense—said that it’s important to have people from marginalized communities, like people without houses or people who use drugs, working in harm reduction. They are subject experts and have a lot of wisdom, and support from within the community itself is particularly important during this difficult time, she told Filter.
The Sidewalk Project currently has three unhoused employees, Snakeoil said. The organization has been around for three years, and offers a slew of services to people who use drugs or live on the street. It is a registered (and mobile) syringe program, hands out naloxone and works to build trust in the community, though the pandemic has brought tricky lines to negotiate between providing services and maintaining social distancing. Workers in the program no longer go into the tents of unhoused people, for instance.
At the same time, in LA, removals of encampments of unhoused people have continued, even during the pandemic. This also makes connecting with the population much harder and erodes a level of trust within the community, according to Snakeoil. “It’s like a public health World War Three here.”
Harm reduction workers across the country are seeing similar issues. The Peer Support Network of New York performs outreach in the city’s homeless community, and offers various other supports such as administering naloxone, and teaching others to do so.
Much like the Sidewalk Project, they have also needed to limit, to the extent they can, close interactions with the communities they work with, while maintaining ties and a level of service. This is hard when homeless people and people who use drugs were already stigmatized and isolated, and part of the program’s importance simply involved interacting with them in a positive way.
“Even before COVID, people were giving them six feet or more,” said Jose Martinez, an active member with the organization. He added that both peers working in the program and people without houses may in some cases have additional underlying health issues, making existing and working in the pandemic even more precarious.
He said the discrepancies were bad prior to COVID-19, but the pandemic has made it worse.
Because many marginalized people lack computers and phones, the Peer Network is a kind of point of contact between them and official public health channels. Members of the organization will regularly share new public health announcements and protocols, and statistics about the overdose and COVID-19 pandemics, said Hiawatha Collins, the organization’s founder.
“We are the first ones to provide them with said information,” Collins said. “Being that we treat them with dignity and respect, we get a lot of information from them too.”
Over the decade or so of the Peer Network’s existence, Collins has seen the labor inequalities between peer and non-peer staff firsthand. He said the discrepancies in pay and ability to climb higher in an organization were bad prior to COVID-19, but the pandemic has made it worse.
COVID-19 has also made it harder to access some of the supplies harm reduction organizations need to operate, such as personal protective equipment (PPE) and needles, Martinez said.
Organization-Level Challenges
Organizations typically plan ahead to get the supplies they need to serve a population of a certain size. But because many harm reduction organizations have had to shut down, many of their clients turn instead to the operations that remain. These may not have stores big enough to cope with the influx, or may have trouble getting more, according to Jennifer Carroll, assistant professor of anthropology at Elon University in North Carolina, who has worked with several US harm reduction organizations.
Further vulnerabilities apply to harm reduction organizations in these times. Many of these organizations operate based on grants, donations or government funding, some of which can be in short supply during a pandemic. This can translate into a money crunch for the organizations.
Harm reduction groups may be understaffed at the best of times, but particularly during the pandemic. And the spaces they operate out of, if they have a brick-and-mortar location, may have little room for social distancing, hampering their work.
In Montreal, a few safe consumptions sites (SCS) have had to close down due to the pandemic. Alexandra de Kiewit is an outreach worker with CACTUS, a remaining SCS in the city, and a co-founder of the Canadian Association of People who Use Drugs.
Back before COVID-19, CACTUS tended to reverse one overdose every one to two weeks, de Kiewit told Filter. However, the illicit-market disruptions precipitated by the pandemic have caused an influx of adulterated drugs, which has seen overdose numbers spike. Last month, CACTUS responded to around one or two overdoses each day.
To make matters worse, the site has had to dramatically alter its operations. Before the pandemic, people could come into the organization’s building, grab materials, access resources, inject on site, then hang out in the organization’s chill-out room. There were, back then, 10 places for people to inject at the same time. Now, due to the need for physical distancing, there are only five.
People also now have to leave immediately after consuming drugs, unless they are too intoxicated to do so. Similarly, if someone overdoses on site—and if naloxone and oxygen fail—everyone without a fitted mask needs to leave the area while staff ventilate, and the room then has to be closed for two-to-three hours to curb potential risk of COVID-19 transmission.
“We can still help people if they overdose, but it’s more complicated,” de Kiewit said.
Though de Kiewit is open about her drug use, she is not a peer worker. In general, she said, peers do a similar job as her, but end up making much less on their paychecks. In some cases, these workers might actually make more going on welfare, rather than trying to live off some of the salaries, she added, and there is still a lot of work that needs to be done until peers are treated as equals in the field. “COVID or no COVID, there’s a thin line between hiring peer [labor], and cheap labor.”
“No one is putting out lawn signs thanking outreach workers, when they really should be.”
When people think of frontline workers in the pandemic, they largely think of teachers, nurses and doctors, not those working at syringe programs or SCS. As such, both material and emotional supports are less likely to come these workers’ way, Carroll said. “No one is putting out lawn signs thanking outreach workers, when they really should be.”
Carroll noted that the pandemic has produced some grim public health failures, but that some jurisdictions have implemented ideas that could help harm reduction more broadly. The expansion of telemedicine programs, the implementation of a safe supply of drugs and relaxation of take-home methadone regulations, for example, have all taken place in parts of North America during the pandemic.
There are also, Boyd said, ways to combat some of the labor inequalities that people who use drugs face while working in harm reduction—a number of them ideas that have gained traction during the pandemic. Decriminalization could destigmatize drug use, and remove other employment barriers for peer workers. A universal basic income would support the peers and make them less likely to go to work if they get sick. More funding would allow the organizations to pay more equitable wages for work that can be draining and potentially dangerous.
“This work needs to be recognized as essential,” she said.
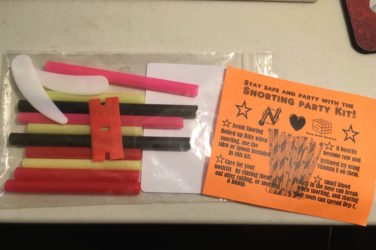
Photograph of a mobile hepatitis C testing set-up in New York City by Filter