In the wake of the COVID-19 pandemic, and in the midst of the overdose crisis, many harm reduction workers are experiencing burnout. While there’s growing awareness of this issue for staff in many fields, like health care, people working in harm reduction and community organizations face a slew of specific challenges, according to a new paper. There are inevitably knock-on impacts for people in need who are served by these organizations.
The paper, published in the Harm Reduction Journal, is based on interviews that Shoshana Aronowitz, assistant professor in the School of Nursing at the University of Pennsylvania, collected in July and August of 2020, close to the start of the pandemic. Immersed in harm reduction work herself, she recalls talking with colleagues about how the pandemic was impacting their work, and how they anticipated it would continue to do so.
Burnout came up again and again. “I was having these conversations constantly,” she told Filter.
From there, Aronowitz decided to collect qualitative data, by speaking with other people about their experiences of working in harm reduction and overdose prevention in Philadelphia, in both paid and volunteer positions. She and a team of researchers then examined the data provided by 30 harm reduction workers, substance use disorder clinicians and community organizers.
“With qualitative data, I feel like you really get into the heart and soul of what people are thinking and how they’re feeling,” Ijeoma Unachukwu, first author of the paper and MD candidate at Rutgers Robert Wood Johnson Medical School, told Filter.
The team coded the results against an existing model of burnout among physicians, which states: “Burnout is a syndrome characterized by exhaustion, cynicism, and reduced effectiveness.”
The model did not include some of the themes found, namely, “concerns about safety at work, lack of control over the work environment, and experiences of task-shifting”
The model includes various factors: workload and job demand, being able to find meaning in the work, control and flexibility, integration between work and life, the culture and values of a workplace or organization, resources and efficiency, and social support and community.
While the researchers’ results paired with many of these factors, the model did not include some of the themes they found, namely, “concerns about safety at work, lack of control over the work environment, and experiences of task-shifting” the paper notes.
Further, existing models don’t apply for volunteer workers, people with lived or living experience of substance use, social workers and “people outside of the traditional health care setting,” Unachukwu said.
Task-shifting was one commonly discussed theme. In traditional health care settings, tasks are regularly delegated to whomever is available during high-stress situations. This isn’t necessarily a burden or an issue, Unachukwu said. It can allow people to explore different roles.
That said, during the pandemic in particular, it became common practice for harm reduction workers to end up “picking up a lot of slack,” or “having undefined roles,” during periods of distress or uncertainty, she continued. “I think in our specific setting, it became a burden, but for all the reasons COVID was a big burden overall.”
Aronowitz added that task-shifting isn’t “in and of itself a bad thing, but I think it can become very burdensome for folks when they feel like they either don’t have the resources, or time to add more things to their schedule.”
Sometimes, workers won’t have been trained to do the things they’re being asked to do. Additionally, harm reduction or community organizations typically face significant financial limitations, and people working in harm reduction often aren’t compensated at the same level as those in other fields for performing similar tasks. All of this can contribute to burnout, Aronowitz said.
The researchers said that these findings could very well apply for other cities—and that certainly appears to be the case.
“You feel guilty for not feeling as sad as you should, or not having enough time to grieve.”
Brittany Graham, executive director and community developer with the Vancouver Area Network of Drug Users (VANDU), said that burnout is commonplace in the field. COVID was one thing, she explained, but the ongoing overdose crisis—claiming ever more lives in communities like hers—makes it increasingly hard to stave off burnout.
“As more and more people die … you feel guilty for not feeling as sad as you should, or not having enough time to grieve,” she told Filter. “But then, sometimes you feel all the emotions for the people. There’s not a lot of space or time for that work, or to remember people.”
In those circumstances, there’s still much work to do, and many people who need help. “It could be your best friend—you don’t have time to grieve,” Joe Raithby, VANDU’s vice president, told Filter. “You’re dealing with other people.”
But the pressures continue to mount. People who use drugs often don’t get adequate care in the formal medical system. Welfare payments in British Columbia are low, and housing costs—including subsidized housing—are increasing, Graham said. Many social services don’t operate at the same level as they once did.
This means that people who use drugs and/or are unhoused will sometimes come to VANDU, which is primarily an advocacy organization, seeking supports they can’t find elsewhere. “If we have a blanket, we’ll give them a blanket. But if we don’t have a blanket, we can’t help them,” Raithby said.
Harm reduction workers and community organizations need to be strategic about where they put their efforts.
In terms of task-switching, VANDU doesn’t have the funding to hire, for instance, a dedicated janitor to do cleaning, so that falls on already-overburdened workers. The same is true for human resources staff, Graham said. These roles simply “become informal tasks that everybody in the organization takes on.”
There are a great many things a person could be doing every day, Graham continued, but never enough time to do them all. So harm reduction workers and community organizations need to be strategic about where they put their efforts. When workers feel like it’s impossible to do their jobs at their best, she said, that can contribute to burnout.
Both the researchers and the VANDU workers said that increases in funding and resources would help address this issue, as it would allow organizations to hire and train more people, and increase their ability to buy supplies. Yet government funding for harm reduction organizations remains limited, Graham noted, and what little there is may be spread across several organizations.
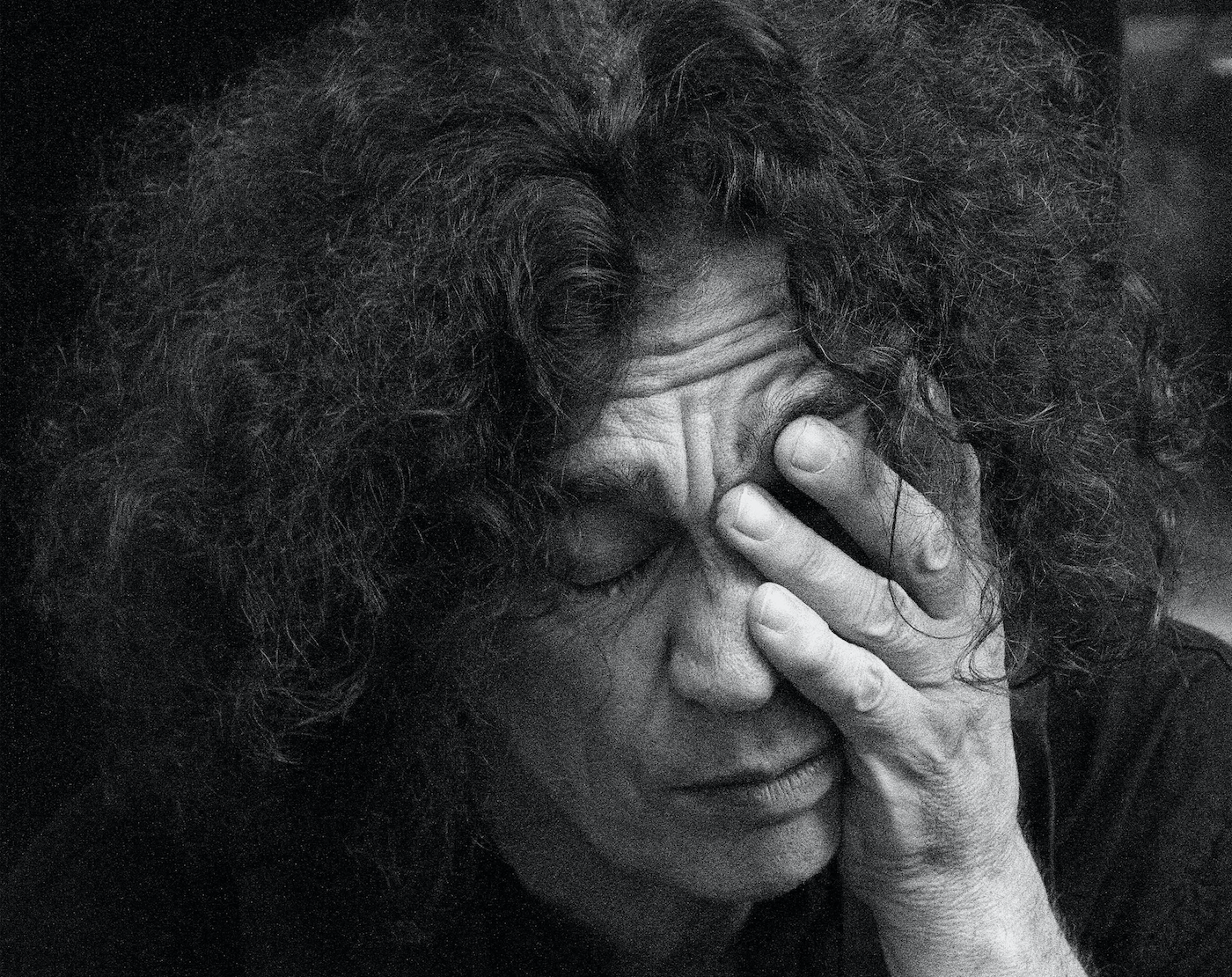
Photograph by Brut Carniollus via Unsplash