Inside supportive housing facilities in Kelowna, British Columbia, residents who use drugs reported that publicly funded health care services were often unavailable to them. In particular, older residents, most of whom are disabled, reported that visiting home health providers withheld care after they discovered signs of drug use. Residents rely on home visits for services related to palliative care, incontinence and bathing.
In August and September 2020, researchers conducted interviews with 42 supportive housing residents and 30 staff from Interior Health, the regional health care authority that oversees public health care in Kelowna. Residents described a pattern of ongoing discrimination—particularly impacting those who use drugs. Many residents reported that after a provider noticed signs of drug use, including cigarette smoking, they were refused the care they needed. The research was published in the May 2023 issue of the BC Medical Journal.
“[Providers] had refused to come into people’s homes due to … cigarette smoke in the air,” lead author Dr. Hannah Gibson told Filter. “One [patient] was refused care because of drug paraphernalia in the home—so, not actively using the substance in front of the worker, but just having that paraphernalia there.”
Kelowna currently has six supportive housing facilities, three of which were included in the research. One had an in-house safe consumption site; the second did not, but did offer supplies like naloxone; and the third did not offer harm reduction services.
The province houses people “according to their needs,” but it’s not clear to what degree people who use drugs are intentionally assigned to the harm reduction-oriented facilities. Nor is it clear to what degree the residents of those facilities who need home health care are actually receiving it.
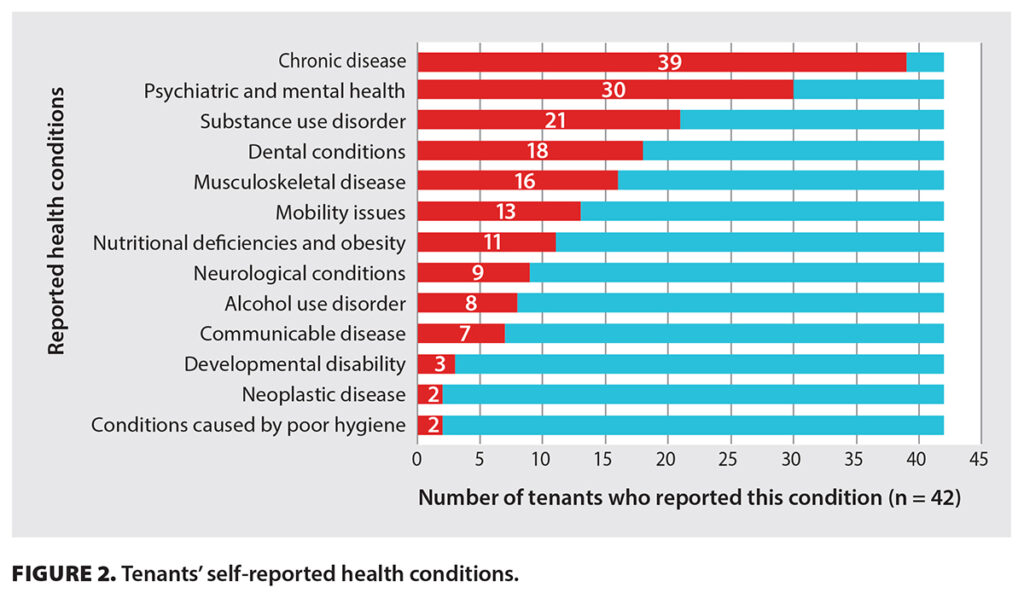
About three out of four residents interviewed require care for two or more chronic conditions, yet only about one-third had accessed Interior Health services. More than half reported not knowing that such services were available. Others reported that they knew, but either could not access the services or weren’t comfortable trying. Interviews with providers yielded similar findings.
Interior Health is one of five regional health authorities in the province, and the only public health care provider for Kelowna. Representatives declined to comment on the reports of staff withholding care, or on their policies related to patients who use drugs; they did, however, email Filter a statement describing the study as “an important body of work” that will help the “address and acknowledge some of the gaps” in its services.
“If you are having a mental health issue that could be substance use related, then you’re turned away from actual support around your mental health until your substance use clears,” one Interior Health provider told the researchers during their interview. “So that’s a problem for most of our residents.”
Dr. Gibson emphasized the importance of health care workers receiving training specific to substance use and behavioral health.
Dr. Gibson, who previously spent a year working as a provider at one of the facilities in the study, emphasized the importance of health care workers receiving training specific to substance use and behavioral health conditions. She pointed to Ellis Place, a 38-unit supportive housing facility that opened in November 2020, as a model—unlike most Kelowna supportive housing, it has in-house staff trained to work with those patient populations.
In addition to specialized training, other measures that the study authors suggested could make services more equitable included expanded hours; mobile outreach teams; and allowing people to opt for “wet” or “dry” housing. None of the three facilities explicitly prohibit substance use, and some residents who don’t use drugs—especially those in recovery—might prefer “dry” housing, just as residents who do use drugs benefit from increased access to in-house harm reduction services.
Both Dr. Gibson and Interior Health told Filter that since the interviews took place, the provincial government has funded more mobile outreach health care services, including a new outreach-oriented primary care unit.
Amid an escalating affordable housing crisis, the population of unhoused people in BC continues to swell. As of September 30, 2022, nearly 1,000 people were waitlisted for supportive housing, alongside another 1,200 applicants to other forms of subsidized housing.
Top image via Crisis Line Association of British Columbia. Inset image via BC Medical Journal





Show Comments