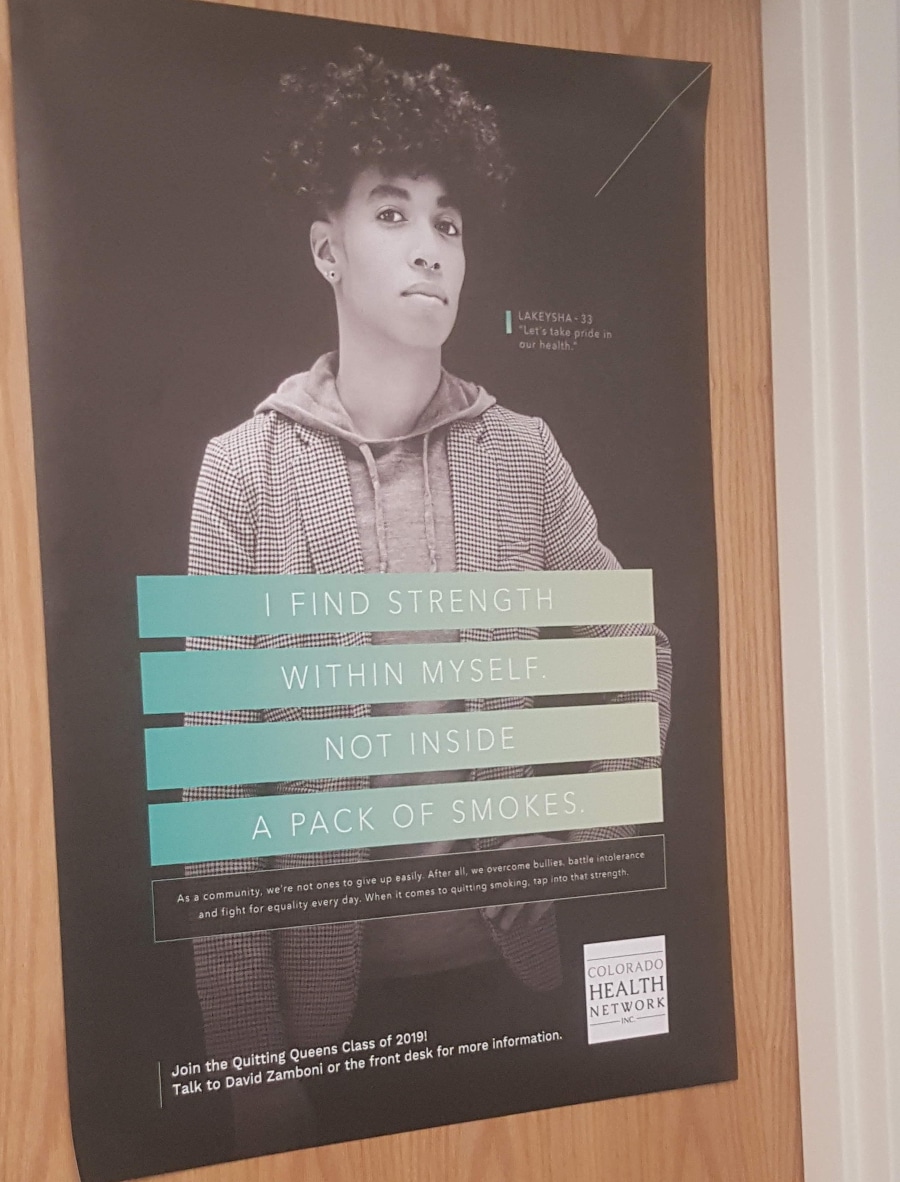
One day last year, when I was working as a medical case manager at the Colorado Health Network, which operates a syringe service program in Denver, I was dismayed to see a poster on the door that echoed “Just Say No” propaganda. It read:
“I find strength within myself. Not inside a pack of smokes. As a community, we’re not ones to give up easily. After all, we overcome bullies, battle intolerance and fight for equality every day. When it comes to quitting smoking, tap into that strength.”
Quitting smoking can be a great thing to do. But was it right for a harm reduction program to proclaim abstinence from nicotine as the only way forward?
Around that time, staff were also asked to sign an agreement that we would not smoke, vape or use smokeless tobacco products within 25 feet of the building. The document outlined the harms of smoking, but added, “E-cigarettes are also a threat as further adverse health consequences continue to arise.”
As a harm reductionist, I was deeply concerned that this program’s policy conflated completely different types of nicotine use—ignoring the efficacy and empowerment of harm reduction for the world’s biggest cause of preventable death.
Regardless, many staff continued to use smokeless tobacco products inside of the building and others would smoke or vape right outside.
“We were asked to make a pledge to not use nicotine products. Nothing ever came of it, nobody enforced it and nobody wanted to sign it,” Sam*, another former Colorado Health Network (CHN) employee, told Filter. However, “When I tried to talk about the potential benefits of vaping and THR [tobacco harm reduction] with my previous manager, they were very dismissive.”
“The overall message was … that vaping was just as harmful as cigarettes.”
A training received in 2019 by program employees—including me—reflected that attitude.
“Around that time there was a lot of panic surrounding vaping and we attended a company-wide training where they incentivized us with food,” Sam related. “The overall message was that all forms of nicotine, except FDA-approved products, were harmful and that vaping was just as harmful as cigarettes.”
“The trainer was an expert in HIV but it felt like they were reading off of anti-vaping material,” Sam continued, “and it was obvious that smoking cessation wasn’t their area of expertise.”
I also recall being given the false information at that event that vaping would cause “popcorn lung.”
When it came to staff speaking with program participants about their smoking, “We were asked to refer people to tobaccofreeco.org, and besides that training we had absolutely no guidance,” Sam said. “When it came to nicotine use, it was never part of the discussion unless someone expressed a desire to quit. We never had conversations about how cigarettes can interact with other drug use.”
Tobaccofreeco.org is part of the CDPHE State Tobacco Education and Prevention Partnership (STEPP). The site erroneously links the “vaping-related” lung injuries known as EVALI with nicotine vaping—even though the CDC belatedly acknowledged in 2019 that Vitamin E acetate found in adulterated THC vaping products was the principal factor.
Filter reached out to the Colorado Health Network for comment about the policy and the training. CEO Darrell Vigil was kind enough to provide a detailed response.
“CHN has not made statements about popcorn lung, e-cigarettes, or vaping, in general,” he said. However, “CHN’s policy does refer to e-cigarettes as a threat.” He then cited the 2018 US Surgeon General’s Advisory on E-Cigarette Use Among Youth, which describes nicotine as an “addictive drug” and states:
“Nicotine exposure during adolescence can harm the developing brain … Nicotine exposure during adolescence can impact learning, memory, and attention. Using nicotine in adolescence can also increase risk for future addiction to other drugs. In addition to nicotine, the aerosol that users inhale and exhale from e-cigarettes can potentially expose both themselves and bystanders to other harmful substances …”
A number of these claims would be contested by experts. They include Charles Gardner, who holds a PhD in developmental neurobiology and is the CEO of the International Network of Nicotine Consumer Organizations (INNCO). “Eighty-nine million American adults are current or former smokers,” he told Filter. “Almost all started smoking in their teens. That’s one third of all adults. If there was any evidence of brain harms [from nicotine], zealous tobacco control researchers would have found it.”
“The claim of ‘brain harm’ is based entirely on young rat studies,” Gardner added. “Changes are not necessarily harms … rat changes morphed into rat harms, which morphed into human harms, which morphed into claims that ‘nicotine is a brain toxin.’”
The point, for harm reductionists, should surely be vaping’s vastly reduced risks compared with combustible cigarettes.
Even the most ardent vaping advocates would not claim that vaping has zero potential harms. But the point, for harm reductionists, should surely be vaping’s vastly reduced risks compared with combustible cigarettes.
Asked about the training where Sam and I received inaccurate information, Vigil said that it was sponsored by a pharmaceutical company, and that CHN had not asked the doctor who delivered it to speak about e-cigarettes.
“It sounds like CHN might be pretty well aligned with Filter when it comes to harm reduction, in general, as well as e-cigarette use as a harm reduction tool,” Vigil added. “We … support harm reduction efforts whether the harm reduction is related to our syringe access program clients, other clients, staff or volunteers. CHN will leave it to the scientific and medical professionals to elaborate on the harmful effects of tobacco and/or e-cigarette use.”
It’s important to highlight that CHN is far from alone in failing to fully embrace tobacco harm reduction. Many other Colorado organizations take similar stances—some of which (unlike CHN) receive anti-vaping funding from CDPHE.
When previously working at the Tri-County Health Department syringe access program, for example, which receives funding from the CDPHE STEPP program, I was also instructed to refer clients who raised concerns about their smoking to tobaccofreeco.org.
“There remains little evidence of less harm from vaping—at least as far as young people are concerned,” Maura Proser, DrPH, the department’s community health promotion manager, told Filter. “In general, TCHD does not promote vaping as harm reduction, as our intention is to treat nicotine dependence. We understand reduced harm steps as part of a step-down process for quitting smoking, which may include nicotine replacement therapy and/or reducing the number of cigarettes smoked in a day … We know there are many cessation aids that are safer than vaping, which is not an approved cessation device by the FDA.”
“Tobacco addiction is a chronic, relapsing condition and recovery is complex,” Abigail Kesner, CDPHE’s communications director, wrote in response to Filter’s request for comment. “CDPHE recommends FDA-approved stop-smoking medications to help people quit smoking … CDPHE also acknowledges that harm reduction strategies can help people. This happens when we meet people where they are, engage them without judgment, and support them in making healthier choices. While vape products are not FDA-approved for smoking cessation, the CDC and CDPHE agree if an adult chooses to vape in order to quit smoking, they should try to switch completely from combustibles to vape products.”
It will be interesting to see whether, and how quickly, the stance of such organizations changes if the FDA determines—as it may do in September under its Premarket Tobacco Product Applications process—that marketing of certain vaping products is “appropriate for the protection of public health.”
It should be emphasized that CHN, TCHD, CDPHE and many organizations with anti-vaping policies, in Colorado and far beyond, do vital harm reduction work in other areas. That’s why their nicotine policies, in comparison, make so little sense.
Why aren’t harm reduction programs universally applying these principles to nicotine, vocally embracing THR alongside other lifesaving initiatives?
As harm reductionists, we know that eliminating harms by simply not using substances isn’t always easy for anyone—let alone for the marginalized populations who disproportionately smoke and have many stressors in their lives. That’s why we focus not only on supporting people who choose to quit, but on promoting access to alternatives with fewer risks. That may look like providing sterile syringes to prevent disease transmission, or medications for opioid use disorder, or a safe supply of drugs of any kind.
At CHN, as a case manager providing services to people living with HIV, I wasn’t instructed to tell clients just to stop having sex. Instead, I was trained to engage in open and honest conversations about their needs, discussing various concepts and options like monogamy, condoms, U=U (undetectable=untransmittable) and PrEP.
So why aren’t harm reduction programs universally applying these principles to nicotine, vocally embracing THR alongside other lifesaving initiatives? For any organization committed to reducing disease and death, it’s the only way forward.
The poster on the CHN door didn’t last too long.
“The sign pissed me off and without talking to anyone about it I just took it down one day because it wasn’t conducive to what we were doing,” said Sam. “Why can’t cigarettes give me strength? It doesn’t take away from your value as a person … Staff would drink coffee around the clock just to do their work. If I instead needed to smoke, vape or chew to work, how is that any different? Shaming someone for the substance they use to ‘give them strength’ takes away from the innate strengths and autonomy participants hold.”
“I often had participants who came into the exchange with their vape and juice … They were like, This is great for me, I haven’t gone back to smoking cigarettes,” Sam continued. “Others would come in coughing, with multiple instances of pneumonia which left them with lung complications, but they always continued smoking cigarettes.”
“Most participants didn’t care about stopping; they wanted their nicotine. If they were offered tools—besides gum and patches, which many participants tried and didn’t like—they would be more able to reduce harms from health complications like pneumonia. As a harm reductionist, I see vaping as another way for people to get the help they need.”
Top photograph by Sophie Riches via Wikimedia Commons/Creative Commons 3.0
*Name has been changed at the source’s request.
Both INNCO and The Influence Foundation, which operates Filter, have received grants from the Foundation for a Smoke-Free World.





Show Comments