Kenneth Anderson is perhaps best known in the harm reduction movement as the founder and executive director of HAMS (Harm Reduction, Abstinence and Moderation Support)—a nonprofit support group with over 9,000 worldwide members who wish to take a harm reduction approach to their alcohol use.
I know him in part through my own work with HAMS. He brings to his role a unique combination of lived experience—he has worked for syringe programs and successfully used harm reduction to change his own drinking habits—and academic rigor, holding MAs in the psychology of addiction and in linguistics.
Besides harm reduction techniques and support, much of Anderson’s work has concerned stigma and abuses inflicted on people who use drugs or alcohol in the name of treatment—again, he has firsthand experience of this, having gone through addiction treatment programs himself.
In this context, he recently published (in two parts) Strychnine & Gold, the first volume of The Untold History of Addiction Treatment in the United States. I wanted to ask him about the book’s purpose—and how history repeats itself in today’s controversies.
Many of us might assume that the addiction treatments of the past were invariably cruel and dehumanizing. Some were. But Anderson’s book shows that other practitioners had a more enlightened attitude. That casts the abusive and humiliating practices that persist today in an even worse light; more optimistically, it suggests that cruelty against people with addiction doesn’t have to be a permanent part of our culture.
April Wilson Smith: What is this book about and why did you decide to write it?
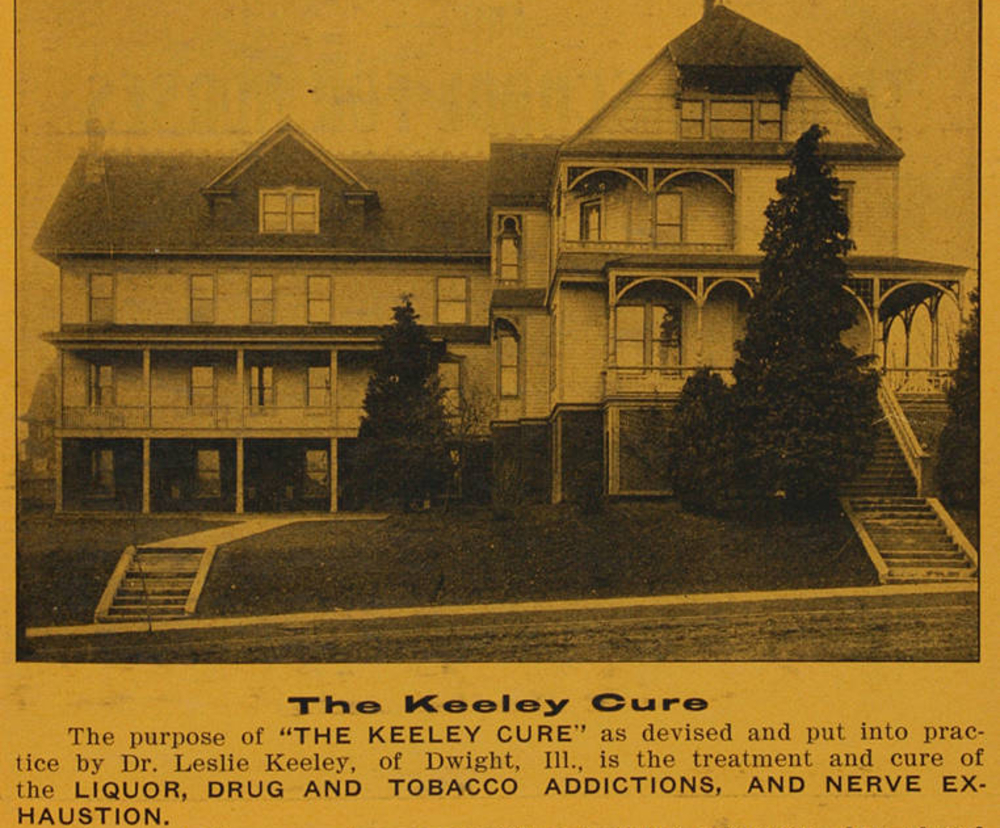
Kenneth Anderson: This volume covers the propriety cure institutes, founded by entrepreneurs who sold “cures” for alcohol addiction, that existed roughly between 1890 and 1920. A proprietary cure is essentially a “secret formula.” The methods of these institutes varied but their philosophy was to get people well and send them on to live their lives—unlike either the “inebriate asylums” of the time or today’s 12-step movement.
It is part of a much longer series about the evolution of addiction treatment in the US from its start to the present. I decided to write this because I wanted to look at the economic forces that led the US to evolve its current, extremely bizarre treatment system.
People who use substances are just people. That has too often been forgotten.
For example—since we know that countries like Switzerland give away methadone, allow doctor’s office and pharmacy dosing and have seen an 80 percent drop in overdose deaths—why does the US still have for-profit methadone treatment clinics that often charge people $400-$500 dollars a month, forcing people to travel long distances and stand in long lines instead of giving them free methadone where it’s safe and convenient? Our system has led to a five- or six-fold increase in overdose deaths over the past 20 years, yet it persists.
In the history of addiction treatment, we can see many parallels with today’s ideological battles. For example, the conflict between 12-step treatment that wants lifelong participation and is opposed to any pharmaceutical assistance and harm reduction forces that embrace whatever methods actually work, some of which are pharmaceutical.
People who use substances are just people; some may have a substance-related problem but are not fundamentally different from other people. That has too often been forgotten.
When did these proprietary cures get their start?
The story begins in 1886 when a number of Russian doctors began publishing stories in medical journals that showed that strychnine injections led “chronic inebriates” (people who drank to excess) to spontaneously stop drinking alcohol. These papers were translated into English and widely published in English-language medical journals.
At this time, treatment for alcohol addiction in the US was basically the monopoly of an organization called the American Association for the Study and Cure of Inebriety. This organization was composed of orthodox physicians who totally rejected the concept of any type of pharmaceutical treatment for alcohol addiction. They believed that inebriates could only be cured by locking them up for years in inebriate asylums. The organization completely ignored this Russian research and did not mention it once in its journal.
People began flocking to Dwight seeking “the Gold Cure.”
Meanwhile, in Dwight, Illinois, an enterprising railroad doctor (a doctor employed by a railway company) and patent medicine salesman named Leslie E. Keeley read about the Russian strychnine cure and decided to give it a try. Much to his surprise, the strychnine cure seemed extremely successful, and his patients stopped drinking.
Keeley, being a very savvy marketer, never told anyone that his injections contained strychnine or that they came from Russia and had been published in medical journals. Instead, he claimed that his secret ingredient was gold, and that he had spent decades of painstaking research developing “the Gold Cure.”
First, news of this spread by word of mouth, and people began flocking to Dwight seeking “the Gold Cure.” Then, in February of 1891, Joseph Medill, editor of the Chicago Tribune, began running articles praising the Keeley Gold Cure and giving it national exposure. Within a few months, Keeley was treating nearly 1,000 patients a day with a battalion of doctors.
Can you describe how the Keeley Cure worked?
The Keeley Cure consisted of injections of very small doses of strychnine and atropine (a belladonna alkaloid) four times a day and drinking a teaspoon full of a tonic (of which the main ingredient was extract of red cinchona bark) eight times a day. In the early days the treatment lasted 21 days; later it was extended to 28 days. (I think that rehabs stole “28 days” from Keeley, but that’s just my personal opinion!)
Patients undergoing the treatment were allowed to drink all the alcohol they wished and were free to come and go as they pleased. The only requirement was that they show up on time for their injections. These elements, and the agency they afforded patients, might be seen as compatible with modern harm reduction approaches.
After about three days of treatment, patients developed a total disgust for alcohol and spontaneously stopped drinking.
To what do we attribute this?
No one really knows. All we have is the empirical data, which was replicated by studies by multiple American doctors, including at the State Inebriate Ward at Rochester, Minnesota. All we know is that after about three days of these injections, patients spontaneously stopped drinking.
It’s difficult to tell what percentage of people stopped drinking permanently; however, it seems clear that a reasonably large percentage did use the treatment as a springboard to lifetime abstinence.
The Keeley Cure was also adopted in the National Old Soldiers’ Homes and for a short period by the US Army. The National Old Soldiers’ Homes were required to keep statistics and were reporting long-term cure rates (meaning total abstinence) of 90 percent.
We are unlikely to get a randomized controlled trial anytime soon.
Another study was done by the Christian Advocate, whose editor had no opinion one way or the other. The editor wanted to know if it was worthwhile to recommend people to the Keeley Cure or not. The Keeley Cure was very controversial because the orthodox doctors were constantly publishing articles in medical journals and the popular press which claimed it was a scam. The Christian Advocate polled clergymen and doctors about people they knew who had taken the Cure. They reported that 50 percent maintained long-term abstinence. Those are our two sources for long-term follow-up.
Needless to say, no one should attempt this method in unregulated settings now. Its apparent efficacy might be worthy of further study, but there’s not really any reason to think that the strychnine cure is better than conditioned taste aversion. We are unlikely to get a randomized controlled trial anytime soon.
Isn’t using strychnine as a medicine a really bizarre idea?
Not really. Nux vomica, seeds which contain strychnine, have been used as a medicine in India since ancient times. Strychnine was isolated from nux vomica in 1818 and was a very commonly used medicine throughout the 19th century and up into the 1920s. Strychnine is a very effective cardiac stimulant. However, by the 1920s, equally effective and far less toxic cardiac stimulants had been discovered, and the use of strychnine as a medicine fell out of style.
This was the time of the Temperance Movement. What did they say about the Keeley Cure?
The Temperance Movement, already actively lobbying for Prohibition in the 1890s, was very much pro-treatment and endorsed all forms of treatment—including both the traditional forms favored by the American Association for the Study and Cure of Inebriety and proprietary treatments like the Keeley Cure.
Contrary to common belief, the Temperance Movement was not about punishing “drunkards”—it promoted Prohibition (enacted in 1920) as a public health law to stop the sale of alcohol. It did not outlaw consumption and purchase of alcohol, only manufacture and sale. Unfortunately, Prohibition backfired when it was enacted, in similar ways to the later prohibitions of other drugs.
Many people who graduated from various cures for alcohol addiction joined Temperance societies and used them as support groups to stay abstinent. The Temperance Movement was very popular, so you got a lot of social support if you didn’t drink.
Did the Keeley Cure spread?
Eventually 126 branches of Keeley Institutes were in operation worldwide, including Great Britain, a Scandinavian branch, Mexico, several in Canada, and elsewhere. Countless imitators also sprang up, some of which were very short-lived. The longer-lasting ones each have a chapter in the book.
What was life like at the various institutes?
The Keeley Institutes did not board patients. The patients all rented rooms in boarding houses. The institutes supplied all the whiskey so they could track how much you drank and did not allow outside liquor. No cigarette smoking was allowed at all, on or off the property, but cigars were allowed up to 15 minutes before your shot. Everyone had to take a bath at least twice a week. No gambling was allowed.
About 95 percent of the clients were men. For women, the doctors went to the women’s residence to give them the injection instead of making them stand in line exposed to public view.
There were no restraints placed on patients socializing, but it was not required. In 1891, several patients got together and decided to form a Keeley Club while they were undergoing treatment. The idea became very popular and soon there were Keeley Clubs in cities all throughout the US, primarily of graduates of the treatment. They supported each other in not drinking and raised funds to send indigent “high-class drunks” to treatment.
There was also a Keeley Club Women’s Auxiliary. It was initially wives of Keeley graduates but rapidly accepted any woman who wanted to help raise money and spread the word. A couple years in, they changed their name to the Women’s Keeley League to broaden their purpose, because they realized that in several places there was a women’s organization but no men’s organization. The Keeley Club membership peaked at 30,000. About half a million people took the Keeley Cure.
Were there other proprietary cures?
Keeley’s biggest competitor was the Neal Three-Day Liquor Cure, which paired emetics (medicines that make people vomit) with alcohol to make people throw up and give them an aversion to drinking. People would be given an emetic roughly at the same time as alcohol, so would develop a conditioned response that alcohol would make them throw up. Today we call this conditioned taste aversion.
In the 1940s it was refined into a science by the Shadel Sanitarium in Seattle, Washington, and published in many medical journals. The Neal Cure was founded in 1909 and approximately 80 Neal Institutes were established worldwide.
Wasn’t the Keeley Cure also conditioned taste aversion?
No. People getting the strychnine injections rarely reported vomiting as a result. The mechanism by which strychnine produced an aversion to alcohol remains unknown.
What happened to the proprietary cures?
Demand for treatment for alcohol addiction largely disappeared in the second half of the 1910s. This could possibly be attributed to World War I. Drinking—or at least getting drunk—had become very unpopular at this point. There were also a number of state prohibition laws in effect, and treatment demand dried up.
The majority of alcohol addiction treatment cures, both proprietary and orthodox, shut down prior to national alcohol Prohibition. A few managed to survive, and the Keeley Institute at Dwight did not close until 1966.
What about the orthodox treatments of the times you cover?
The orthodox cures were at state-run inebriate asylums, private hospitals and sanitariums and inebriate homes. This is the subject of volume 2, but as a preview, at the Foxboro State Hospital in Foxboro, Massachusetts, patients were committed for two years. Their therapy consisted of farm labor and gymnastic exercises; religious services were held on Sundays, and about every other week they had an educational lecture on such topics as “The Hawaiian Islands” “Japan and Its People” or “The Earthworm and its Work.” They also gave musical entertainments.
Were the “inebriate asylums” locked down the way today’s rehabs are?
At Foxboro, one of the wards was locked. The other was not locked, but people were not free to come and go—they were incarcerated. The open ward was for people they thought would not run away.
If you worked on the farm and did your gymnastic exercises faithfully for six months, you got out on parole. If you stayed abstinent until your two years were up, you were free. If you got drunk again, you got sent back to hospital.
The court system initially sent people to these places for public drunkenness, drunk and disorderly conduct, domestic violence while drunk, etc. This kind of behavior, prior to the existence of inebriate asylums, would have gotten you sent to jail, but for a much shorter period than two years.
Did the proprietary institutes change public perception of people with drinking problems?
They convinced a lot of people that addiction was a curable disease. Keeley wrote a book called The Non-Heredity of Inebriety, which proposes many ideas of the modern disease theory. The title is misleading because Keeley believed that there could be genetic predispositions to alcohol addiction, but what he was rejecting is degeneration theory. Degeneration theory was based in Lamarckian evolution and proposed that acquired traits could be inherited, as opposed to Darwinian evolution, which said they’re not.
Keeley said that normal people who have this habit can be cured—they’re not fundamentally morally corrupt.
According to degeneration theory, if someone became a “drunkard,” they would pass down drunkenness to their offspring, who would give birth to “thieves,” “idiots,” etc., which would lead to the end of the line. T. D. Crothers, the de facto leader of the Inebriate Asylum movement, was a believer in degeneration theory.
Keeley said acquired traits were not passed down. He said that normal people who have this habit can be cured—they’re not fundamentally morally corrupt.
Were there any negative long-term health effects of the Keeley Cure?
The people who ran the inebriate asylums said the Keeley Cure made everyone “insane” and that they ended up in asylums, but at the Soldiers’ Homes, out of 600 people who took the Keeley Cure, only one went to such an institution—the same rate as the general population. There were no actual reported long-term side effects.
Why do you think no one does conditioned taste aversion now?
They are still doing it at Schick Shadel hospital. There was a big chain in the 1980s of aversion treatment hospitals called Raleigh Hills. The National Institute on Alcohol Abuse and Alcoholism (NIAAA) was run at the time by 12-steppers who hated all non-12-step treatments, so they targeted Raleigh Hills to shut them down in the mid-1980s; unfortunately, the NIAAA caught Raleigh Hills double-dipping from Medicare. This was a scandal reported in the LA Times and other newspapers in 1982.
No doubt 12-step rehabs also double-dipped from Medicare, but they weren’t being targeted from Washington. That was the end of any large-scale aversion treatment in the US—all due to politics, nothing to do with science.
Detail from a 1909 Keeley Institutes advertisement via Wikimedia Commons/Public Domain




Show Comments