On July 12, the Centers for Disease Control and Prevention published a report that found an “encouraging” increase in recent years in urban-living queer men’s awareness of pre-exposure prophylaxis (PrEP).
This HIV prevention medication reduces the risk of getting HIV from sex by over 90 percent—and the risk of transmission via injection drug use by 70 percent. But in some of the cities covered by the CDC’s report, many people who inject drugs are wholly unaware of the “miracle drug,” as HIV activists have dubbed it.
From 2014 to 2017, 20 cities saw PrEP awareness among men who have sex with men (MSM) skyrocket from 60 percent to 90 percent. Additionally, MSM’s PrEP use increased from 6 percent to 35 percent.
While 82 percent of surveyed Baltimore MSM knew about PrEP in 2017, only a quarter (24 percent) of surveyed syringe exchange participants, in 2016, were aware of it. Even more starkly, nearly all (96 percent) of surveyed Boston MSM were familiar with PrEP, while only 12 out of 33 Boston injection drug users had ever heard of it.
“There just aren’t many public or private investments being made in getting accurate PrEP information to people who inject drugs,” says Angela Bazzi, an assistant professor at Boston University’s School of Public Health. As a result, “MSM patients are more familiar with PrEP because it might be more talked about and known,” one Boston physician told researchers. “But our patients who inject drugs are very high-risk as well.”
In 2016, 9 percent, or over 3,000, of the nearly 40,000 HIV diagnoses in the United States were for people who inject drugs (PWID), even though only 1.4 percent of women and 2.6 percent of men in the US have ever engaged in injection drug use.
The often-fraught relationships between PWID and physicians can mean the difference between a patient accessing PrEP or not. For one, PWID can feel stigmatized by their doctors and, in turn, choose not to disclose their use: “I hate telling the doctor that I use drugs … because they are going to blame anything wrong with you on the drug use,” says Donna, a patient from Providence, Rhode Island.
Additionally, clients and clinicians alike may not prioritize preventing HIV. For people with substance use disorders, their use “come[s] first,” as Patrick, a PWID from Providence, says. Doctors may consider “their main concern when they are looking at an [injection drug user]” to be connecting them with substance use treatment, explains a program manager of a Boston community-based organization. “No one’s really thinking, ‘Okay, but they also have all these high-risk sexual behaviors that are just as important as their injection behaviors that everyone’s talking about.'”
As seen with engagement efforts and clinical interventions, PrEP use by, and efficacy amongst, PWID is not afforded the attention of scientific research. Only one study, conducted in Thailand, has looked at the efficacy of PrEP for PWID. As the sole investigation into this issue, the Bangkok Tenofovir Study found that PrEP cut the risk of HIV acquisition by nearly a half (49 percent) amongst 2,413 Thai injection drug users.
“Very little is known about the acceptability or accessibility of PrEP for HIV prevention among PWID in North America where PrEP is recommended for PWID,” explain Boston-based researchers in a Harm Reduction Journal study, “but actual uptake in this population has been low, and knowledge, acceptability, and potential adherence challenges remain poorly understood.”
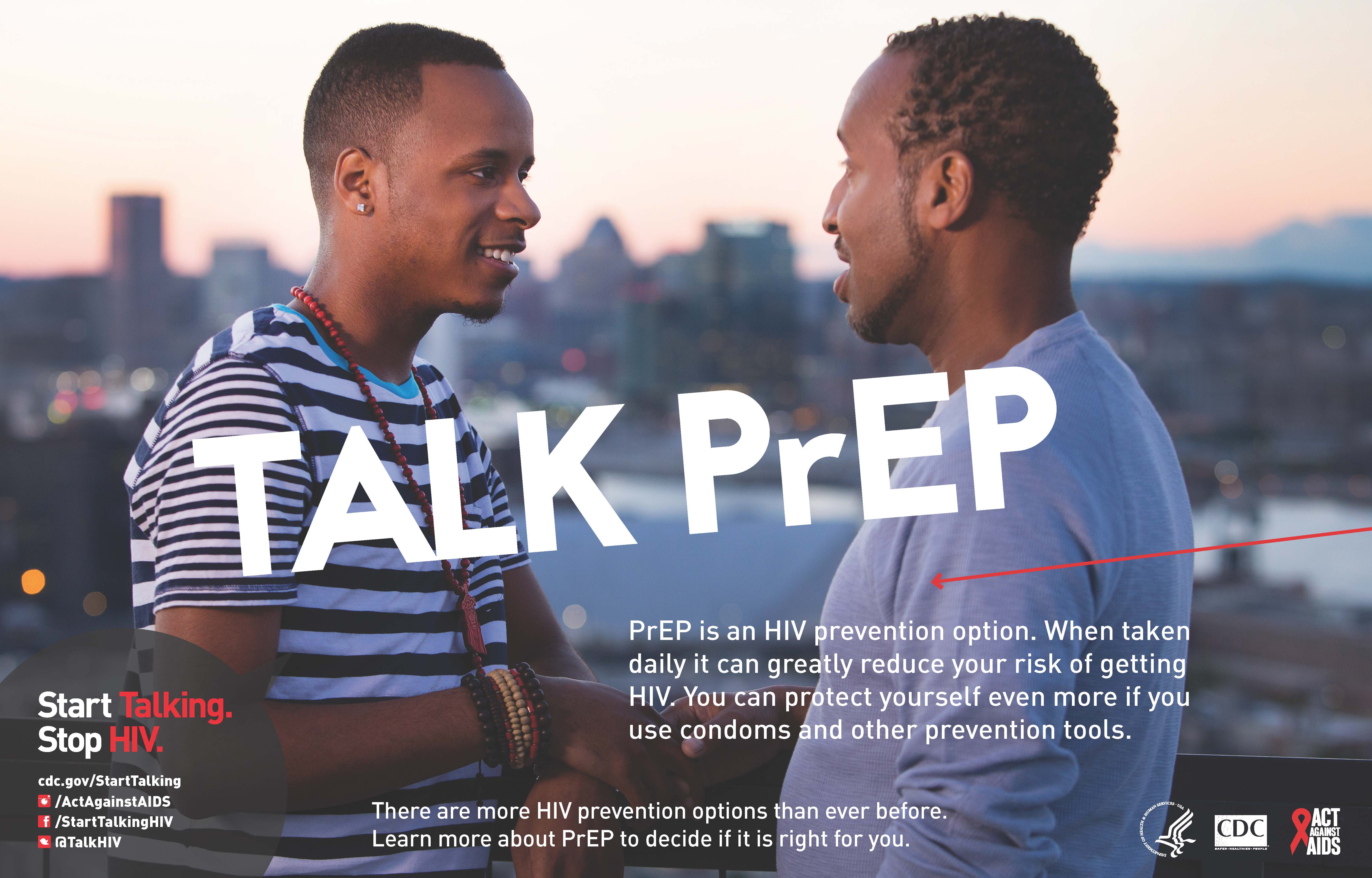
Poster by the Centers for Disease Control and Prevention




Show Comments