[This article is an adapted excerpt from On Opium: Pain, Pleasure, and Other Matters of Substance, which was published in Canada by Goose Lane Editions in September. An audiobook will be available worldwide in 2022.]
With my head forced forward and down, my pelvis forced forward, I suck in my stomach in an attempt to imitate a normal spinal curve and hold myself up. My legs move stiffly. My spine feels unstable. All in all I feel lumbering, ugly, deformed. Monstrous. Every second involves concentration to stay upright. Suffering, what it does to my body, what it does to my mind, and the effort required to transcend it: All of these things make me feel like a monster.
Monsters: They live in books, under beds, and, to my mind, in museums. These days, museums are often bright, slick edutainment machines. It was different when I was a kid in the ’80s. Back then, going to the Royal Ontario Museum in downtown Toronto involved a thrillingly dark subway trip that brought us to a romantically dusty collection of mysterious artefacts from both the natural world and human culture.
As an adult I studied biology and got to know the range of hominid skulls very well in a physical anthropology class. In comparative vertebrate anatomy I came to enjoy dissections, where you can actually see and compare the intricate, individual inner workings of the creatures endowed with mu-opioid receptors (all the creatures with backbones, as you’ll recall). And then I married into a Mexican family and learned to see joy in merry depictions of skeletons and skulls. But as a child then, my fear of monsters and most especially skulls was very real.
In fact, most likely it was to challenge the remaining traces of that fear that I enrolled in the kind of biology courses where you get your latex-gloved hands sticky. And well that I did, because bones have become very significant in my life.
By the time I stepped into a rheumatologist’s office, I’d lived a summer of secret horror.
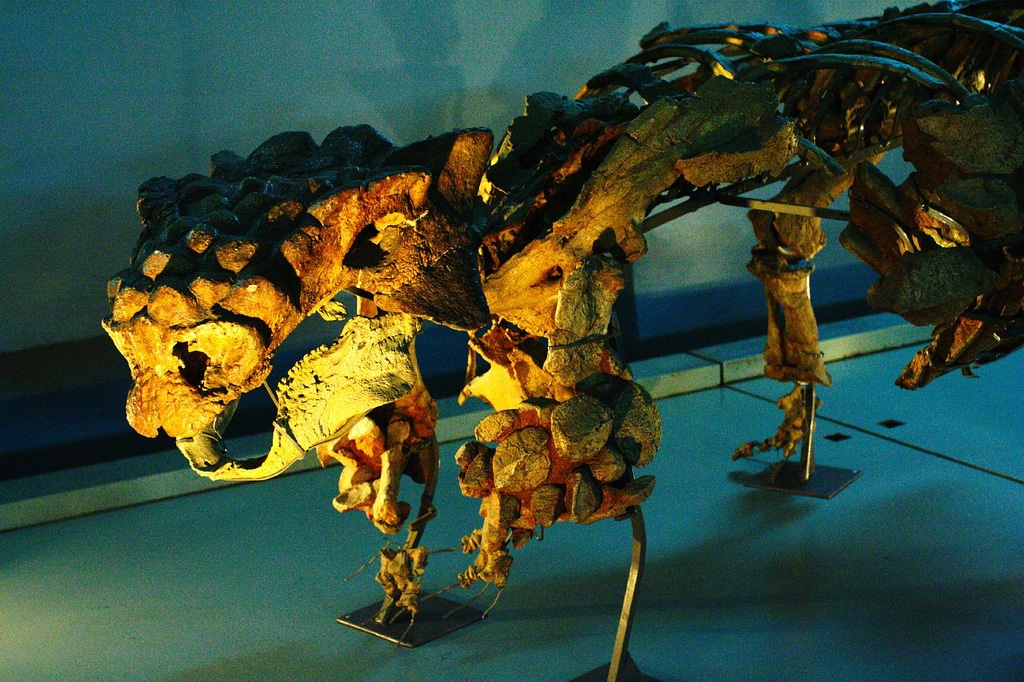
The ankylosaur is a turtle-shaped dinosaur with armoured plates and, in one species, a spikey club for a tail. At some point in my teens, I happened to see a picture of an ankylosing spondylitis patient in a book somewhere. I have a knack for remembering random, useless stuff. And I had seen the ankylosaur at the museum. The dinosaurian name of the disease, the monstrous way the patient was bent over by his condition, back hunched, the bones ankylosed, or fused, just like the dinosaur’s.
When, after my first child was born, I experienced the very distinctive AS pattern of stiffness and pain relieved by exercise, and when lab results suggested a form of inflammatory arthritis as a likely cause, the twin images of that ankylosed patient and the ankylosed dinosaur rose up from my memory vault.
By the time I stepped into a rheumatologist’s office, I’d lived a summer of secret horror, using the internet to retrieve endless images of patients deformed by the bone disease I already knew I had. That September, I held my breath as the rheumatologist diagnosed me with AS in a matter of seconds, told me irritably when I tried to ask questions that, “Well, it’s not going to kill you,” and walked out of the examination room, leaving me reeling, and with a prescription for anti-inflammatories that ultimately burned a hole in my esophagus.
Over the years, I’ve adjusted a lot. And now, in the same way I make a pilgrimage to Frida Kahlo’s house when in Mexico, I visit the museum here in Toronto—no longer dusty and romantic, but still full of wonders—on a special pilgrimage to see Zuul crurivastator, “destroyer of shins,” a beautifully preserved skeleton representing a new species of the beast who nearly shares the name of my disease.
Like Zuul, I try to stand up straight but instead curve forward as if my vertebrae were already fused into one bumpy carapace. I try to push my rib cage forward where it belongs but it sinks back, instead bulging into a curve at the back where no curve should be unless your name is Zuul. The gentle C-curve of my neck is flattened out, as an X-ray confirms. Still, the slow deformation of my spine appears to be sparing me the full question mark shape of the untreated AS patient, for whom surgery may be required to allow for a forward rather than downward gaze.
When my doctor wrote a letter to the federal tax agency on my behalf, describing the worsening deformity of my back, the word weighed on me for days. I catch my reflection behind the dance instructor as I move stiffly through a Zumba class and see myself as Quasimodo.
When tramadol is not at its peak effect, I project tension, anxiety, or discomfort—and constant frustration—making me quiet, edgy, and drawn. I don’t know how to tell people what I need, and my many attempts to do so clearly and gently have rarely improved my relationships, instead leaving me more exhausted and more alienated.
Because I’m able to not only walk but run, it is hard to translate the fact that I cannot stand in one spot for more than a few minutes without discomfort curdling to pain into an understanding that I am dealing with a disability. Acknowledging this, as I am gradually beginning to do, means I can start to see that which enables me to do things despite pain as a tool or accessibility aid, and my ability to access it as an element of disability rights. Still, I often feel misunderstood and shut out of regular life because even though I can enter it, I can’t do it with the constant smile that lets others feel comfortable.
The Casual Demonization of Drug Users
It occurs to me that in journalism, and in casual speech, we often “monsterize” human beings, conflating the physically non-conforming with perpetrators of morally unspeakable acts, by describing both as monsters. Zuul, like other artefacts of nature, is a morally neutral monster, but he or she shares the term in popular thinking with serial killers, animal torturers, child abusers, and people who use drugs.
On Twitter, I have found other monsters: pain patients like me who are all too often characterized as strident, demanding, grotesque, and difficult, gross stereotypes of the barely literate, endlessly consuming American. And then, despite the fact that a psychoactive substance, like a dinosaur, is morally neutral, when certain people use drugs they get the full monster treatment, making it impossible to recall that we are describing a human being, and often one in pain. Drugs journalism, or pulp horror fiction? It can often be hard to tell. Take this real news article, for example:
OPIOID HELL: The Zombies of a USA City with a Hopeless Addiction That’s Set to Come to UK
A city ravaged by an opioid epidemic last night gave a chilling warning to the UK.
And indeed, you can find these zombies—monsters by definition—lurching in the street; you can find them skulking in the doorways. You can find them crowded into shelters or loitering in parks.
The stereotypes we hear about people who use illicit drugs are atrocious. Like all stereotypes, they are malleable, changing through the years. Rather than the drug being criminalized, it is actually the people who use it who are maligned, defamed, and criminalized through drug laws.
My friend “Joe” is a convicted felon who at 19 spent eight months in the clink, followed by house arrest and probation. We have talked about that, but these days spend more time—through detailed, nearly daily emails, mostly—discussing homelessness, cats, the way Toronto is changing in tandem with other big North American cities, and our shared experience of chronic back pain. We first discovered an affinity on Twitter and began chatting privately.
Joe never asks me direct personal questions, although he’s a good listener who seems to really care about the answer when he asks how I am. Nor does he ask to meet once we discover that we both live in Toronto. But he’ll check in discreetly, if I disappear for a few days, with a gentle “how’s by you?” Nothing more. He answers all of my questions, though.
Joe’s life story has been a nightmare, with many terrible details I won’t share here, because he has become my friend, not my subject. There is no romantic or sexual subtext here: He is in a very committed relationship which, after a decade when his beloved cat was his only companion, has given meaning and purpose to a life previously shot through with despair.
Over the course of months of sporadic conversation, Joe becomes my most regular correspondent after my mom. We meet in person for the first time, at my suggestion, in a café where I used to hang out during university. I moved into my university residence the year Joe moved into the Don Jail, a now-defunct, notorious Toronto institution that looked, he says, like the set of a horror movie. I remember standing outside it for some article I wrote years ago and he is right, but of course I never saw it from the inside.
Joe knows this café too. He spent time here when he was a teenage drug dealer, selling marijuana and LSD at his high school around the corner. That school happens to be where my son has just started grade nine. We are exact contemporaries, born a few months apart, and so we have shared cultural touchstones and memories of the city.
“We’re the junkies,” he writes to me. “Doesn’t that say it all?”
Joe lives now, with his partner, in Toronto’s Gay Village. They live in rent-controlled Depression-era red-brick housing that he describes as a revolving door of “dead-ender” tenants and the odd student from smalltown Ontario, stunned to have ended up smack in the midst of urban decay. “We have some wild tenants around here,” he writes. “I mean wild as in feral, barely domesticated, probably struggling with housebreaking.” His neighbour on one side calls the rooming house on the other side the Murder House. Joe keeps a large combat knife by the door in case someone breaks into their unit.
He recently helped the property manager cart a deceased tenant’s possessions to the curb. Joe suspects the tenant died of an overdose. He describes drug deals taking place nightly in the alley behind his house and picks up discarded methamphetamine and fentanyl needles (he can tell the difference) to keep the place clean and safe. They have had bedbugs. The apartment is actually falling apart, and whenever it rains Joe and his partner must run around plugging holes. They’ve flooded so often they now store their possessions in plastic containers. There’s nowhere else to go.
“We’re the junkies,” he writes to me. “Doesn’t that say it all?”
Joe has not, however, ever injected drugs. His partner is a younger trans man who was injecting heroin when they became neighbors, and who transitioned to the addiction medicine buprenorphine after friendship sweetened to love. Having survived abandonment, domestic violence, dislocation, incarceration, and poverty, so far, Joe’s main focus now is on keeping his little family—which still includes the great orange cat he rescued from under a truck as a tiny ball of fluff—well and whole.
Joe may have dabbled in drug dealing as a very troubled teenager, but he did not come to opioids until adulthood. Upon leaving prison, the only work he could get was manual labour. This exacerbated back problems and, as was common in the ’90s, he was prescribed opioid painkillers. They not only allowed him to continue to work his backbreaking job, but he quickly discovered that, especially when insufflated (snorted) rather than swallowed, they also provided a calm he’d never experienced, a normalcy. With OxyContin, he was at last able to manage his debilitating symptoms of chronic post-traumatic stress syndrome.
Punishing People on Addiction Medications
When prescription opioids became impossible to obtain, Joe made a fateful decision to avoid the unpredictable illicit market. By seeking a safe source of (non-euphoric) opioids through the addiction treatment system, he has been made to take on the stereotype of the junkie, the monster in flesh and blood.
“People think of methadone patients,” Joe tells me, “as dirty, zombielike shuffling semi-humans already crawling with disease. They have a poor sense of who actually goes through clinics.”
To get the medication that keeps him well, Joe must travel to a distant Toronto suburb, where his methadone clinic is hidden behind an auto body shop. By the time he arrives there in the morning to stand in line or squeeze into little waiting area, he is in serious withdrawal, sweating and shaking. Every week, he must provide urine samples. Joe sends me photos that he took from inside the bathroom where he must pee in a cup (in the US, this process often involves observed screening). Although at least he is allowed to lock the door, there are four cameras, some fixed at groin level, to ensure he does exactly what he’s told.
Piss tests are just one, emblematic example of the way vulnerable people are routinely dehumanized and re-traumatized in the name of treatment.
The writer Elizabeth Brico, in Florida, experiences a similarly dehumanizing process when she undergoes witnessed urine drug screening as a requirement for receiving buprenorphine, one of the two most evidence-based treatments for opioid use disorder: “She watched, annoyed, while I pulled up my panties, tugged down my skirt, and sidled past her out the bathroom, empty cup in hand.”
Ultimately Brico relapsed with heroin as a result of her inability to pee under scrutiny.
Although some clinicians claim there is a safety value to patients in knowing what’s in their urine, the tests are notoriously unreliable and easy to mess with despite the punitive precautions, and there is no evidence that they improve patient care in any way. They allow doctors (even in singlepayer-healthcare Canada) and laboratories to bill, often exorbitantly, for provision of the test, and in fact constitute an entire industry devoted to surveillance and reporting of the contents of people’s piss and marketing of ever-more-creative ways to monitor human fluids. These include new, privacy-shredding ventures such as apps4 that allow for observed, recorded alcohol and drug screening.
Philadelphia harm reduction advocate Bill Kinkle, a former nurse who was addicted to heroin, also describes the trauma of this dehumanizing practice, in which he has regularly been forced to relive the helplessness of past sexual trauma and incarceration, including being raped in prison, as part of mandated addiction treatment. Never, he says, has his urine screening been witnessed by an observer of the same gender. He wrote to his case manager under Pennsylvania’s nurse monitoring program,
I want to be as clear as possible here so there is no confusion. What happens every time I am selected for a screen is intense anxiety, cold sweats, an overall psychological heaviness. While I am preparing to go into the restroom I begin to shake and sweat more, most times I joke with the staff to cover the growing impulse to cry and leave the facility, while in the restroom I can smell the jail cell the night I was raped. I can feel the texture of the wool blanket over my face and hear the muffling of sound. My heart races, my voice cracks, and I have to work extraordinarily hard not to spill the specimen as I hand it over because I shake so profusely.
Piss tests are just one, emblematic example of the way vulnerable people are routinely dehumanized and re-traumatized in the name of treatment. As it turns out, whether in treatment or actively using, to most people, you’re a junkie for life, or at least for as long as poverty keeps you neatly slotted into their mental category of the worthless, untrustworthy, unredeemable drug user.
A Violently Racist Narrative
The media-propagated narrative has been that innocent, naive (white) people are prescribed a painkiller and quickly find themselves hooked, ultimately turning to heroin, the true maker of monsters. But people like Joe complicate the reality. So too do statistics on prescription opioids and heroin use. Or the fact that, despite common denial of appropriate opioid pain care to Black patients with serious conditions like sickle cell anemia and other pain conditions, the rates of overdose are now increasing more quickly in the Black community than anywhere else.
It is perhaps natural that pale and privileged people like me would have trouble separating the cause of suffering and its effect. We have a vested interest in not doing it very well. The language of monstrosity that exists so often around drug use reflects the position that certain drug users hold in society and tells us that drug use is deviant, unmanageable, foreign or even alien, and frightening.
The tight connections between white supremacy and the War on Drugs run the gamut from the scapegoating of Chinese immigrants in Canada by means of the first opium prohibition laws, to targeting of Indigenous people for enforcement of minor drug crimes today, or the persecution of Black heroin users. The vocally anti-racist jazz singer Billie Holiday, for example, was hounded by Harry Anslinger, the notoriously racist head of the US Federal Bureau of Narcotics in the 1930s and prime mover of the War on Drugs that endures today in much the same form he first laid out.
More recently, media are quick to report the drug status of Black people killed by police, and police are just as quick to cite drug use or sales or suspicion of either as justification for indefensible and apparently racially-motivated violence.
Since the very start, prohibition, or harsh enforcement of it for certain drugs but not others, have targeted racialized minorities with stereotypes and exaggerations, monstrifying different ethnic groups.
In 2020, for example, we were told that drugs were relevant in the death in Minneapolis of 46-year-old George Floyd, who had a non-lethal dose of fentanyl in his system when a police officer knelt on his neck for nearly nine minutes, as he called for his mother and repeated that he could not breathe; or in that of 26-year-old Breonna Taylor, who was shot six times in her own Louisville apartment during a drug investigation.
Over and over since the very start, prohibition or harsh enforcement of it for certain drugs but not others—often even versions of the same drug, as with the chemically identical drugs crack and cocaine—have targeted the racialized minority associated with it, with stereotypes and exaggerations monstrifying different ethnic groups: crack babies, Yellow Peril, drunken Indians—these are all racist constructions that have nothing whatsoever to do with the actual harms of the drug in question.
The racially associated danger of the drug often has to do with either loss of control or insidious control. Where ruthless Colombian and Mexican drug lords mastermind the enslavement of innocent Americans with cocaine, sly Jews control the legal pharmaceutical opioid industry.
In Robert Louis Stevenson’s story of Dr. Jekyll and Mr. Hyde, a medical doctor “swallows a potion that transforms him from a rational, intelligent human into an evil monster,” write two veterinarians with PhDs in American Veterinarian magazine. The article where this appears is about how to recognize the pet owner who is using their dog or cat to score opioid painkillers—for themselves. “Opioids—the modern equivalent of the doctor’s potion—can create dependency, transform people into strangers sometimes given to harmful deeds, and bring on the distinct possibility of death,” they continue.
For family members whose loved ones have become “strangers sometimes given to harmful deeds,” it can be seductive to describe the drug as such a potion, creating a split personality and turning a beloved child, sibling, or parent into a monstrous creature who exemplifies characteristics like selfishness, manipulation, deceit, and unreliability. “When she’s on drugs she’s just a monster,” says A.Y., mother of a young woman who uses methamphetamines. An FBI feature film purportedly about drug users’ experiences includes a composite user musing on his experience with oxycodone 80s.
It just turned me into a monster. I never thought any of this would happen to me. I’m a criminal. I’m an addict … the minute that chemical hits your bloodstream, you lose control of what it does in your body. You can’t control it. Nobody can control it. And I ask them, of all the drugs they’ve ever tried, what’s the most addictive drug. And without a doubt it’s oxycodone.
Others have said the most addictive drug—without a doubt—is heroin; cocaine; crystal meth; or nicotine. Time magazine reports on a scary new drug (it’s always a scary new drug) based on the opioid codeine. It’s called krokodil, or the “zombie drug” (there are many zombie drugs). It comes from “Siberia and the Russian Far East,” and it is the “world’s most dangerous drug,” causing necrosis of the skin. And, of course, “There are now alarming stories that the monster could be at large in the US.” Other scary “new” drugs that have each had their turn in the tabloid sun have included flakka, bath salts, monkey dust, jenkem, Tik, and Gray Death.
Inevitably, reports like these prove to be nothing but alarming monster tales: moralistic, based on fantasy, intended to scare. When I was a child, we feared that our Halloween candy was laced with LSD (it was not). Now, drug users are apparently giving away cannabis edibles in order to get our children stoned or psychotic (they are not).
The Real Monster
With monster language comes suspicion, vigilance, xenophobia, and fear. Monster language serves, repeatedly, as the scaffolding that holds up discrimination and routine rights violations. The moral of the story is that monsters are not to be trusted: They must be quarantined, killed, institutionalized, silenced. Exterminated. Reporter Susan Zielinski quotes Alberta resident Symantha DeSchiffart on a drug user:
He’s walking like he doesn’t have any bones. He’s right messed up. It’s scary. He’s trying to talk. You don’t know what they’re going to do when they need money. This right here is a zombie apocalypse in this area. It’s not safe for anybody.
The result of commentary like this in this particular community has been closures and defunding of existing supervised consumption sites, moving drug use from a safe, supportive location to alleys, parks, and Burger King bathrooms and resulting in preventable death.
At its worst extreme, framings that effectively reduce people who use drugs to zombies propel regimes like that in the Philippines, where President Rodrigo Duterte openly questions whether drug users are human (his drug war policies and support for extra-judicial killing have resulted in the deaths of tens of thousands of members of the urban poor, with poverty and drug use being repeatedly conflated and subject to similarly hateful and dehumanizing descriptions by the president). Shortly after coming to power in 2016, Duterte told reporters that “Hitler massacred 3 million Jews. Now, there are 3 million drug addicts … I’d be happy to slaughter them.”
According to French economist Thomas Piketty, inequality in the United States is “probably higher than in any other society at any time in the past, anywhere in the world.”
Donald Trump, an open admirer of Duterte’s approach to drug policy, and his militarism and authoritarianism, likewise advocated capital punishment for drug dealers, while using both “animals” and “drug dealers” to refer to Hispanic migrants and renewing the truly undying global War on Drugs. The cost of media recklessness in reporting on drug use without picking apart the racism and poor-bashing inherent in these framings is the cost of human lives.
We—or rather, the wealthy minority who control access to land, resources, services, perspectives—have put together a Frankenstein’s monster of a society. In North America, the gap in incomes between rich and poor is worse than in 1913 Europe; globally, the wealthiest have commanded a greater share of incomes, as well as overall wealth, since the 1980s, and market forces play the tune to which we must all frantically dance. According to French economist Thomas Piketty, inequality in the United States is “probably higher than in any other society at any time in the past, anywhere in the world.”
That’s the society we live in, a true monster with every condition necessary for poor mental and physical health, physical pain, addiction, and misery. Like Dorian Gray, whose face remained pristine while his hidden portrait accumulated all the monstrosity of its subject, or like Frankenstein’s monster, the creation is thought to have all the bad qualities that are in fact the worst qualities of its maker—in fact, if anyone were to listen, it is more eloquent and humane than its creator. We punish this poor beast of a society for lumbering around, seeking shelter, medicating its pain, worrying its own tail, doing its best to live and find its own meaning and beauty.
Really, who is the monster?
Photograph of an anklyosaur skeleton by Thomas Vandenberghe via Wikimedia Commons/Creative Commons 2.0
This article is an adapted excerpt from On Opium: Pain, Pleasure, and Other Matters of Substance, which was published in Canada by Goose Lane Editions in September. An audiobook will be available worldwide in 2022. You can read more about the book, and the author’s other writing, at www.carlynzwarenstein.com.




Show Comments