Viewed from the United States, Canada’s comparatively liberal social mores and universal healthcare would seem to set the stage for some kind of polite, frozen harm reduction paradise.
Indeed, our responses to an overdose crisis as bad, proportionally, as in the US have been both innovative and pragmatic—measures range from Health Canada’s recent approval of injectable prescription hydromorphone to treat opioid use disorder to Good Samaritan laws protecting overdose 911 callers from prosecution. While Donald Trump’s Department of Justice fights the opening of safe consumption sites (SCS), we have dozens of them.
True, the Canadian response still falls badly short of the safe (decriminalized or legally regulated) drug supply and low-barrier, evidence-based addiction treatment which advocates demand. Still, harm reduction policies may even be slowing the long–accelerating overdose rates in Vancouver, on our west coast (there were four suspected overdose deaths there the week I wrote this and five the week prior, compared to a weekly average of seven in 2018).
Vancouver, British Columbia hosts our oldest SCS, Insite, which was founded in 2003 and permitted to remain open thanks to a successful 2008 legal challenge to the previous, Conservative federal government. The city, with its 10-block Downtown Eastside area of deep poverty and open drug use, is both the epicenter of opioid addiction and overdose in Canada, and an area with the country’s highest concentration of harm reduction services, scrambling to keep up.
A Grotesque Social Experiment
But I live over on the other side of the country, in Ontario—a province over one-and-a-half times the size of Texas with a population of over 14 million, 6.3 million of whom live in the Toronto region. Belatedly anticipating the eastward spread of fentanyl and now carfentanil, we copied many of British Columbia’s innovations, although not at the scale needed. Still, it was a start.
Until, that is, we elected a new provincial government late in 2018.
Swift, brutal policy and funding changes broadly in line with Thatcherism or the US Republican Party.
Our new premier is right-wing populist and millionaire Doug Ford (brother of the late Rob Ford, best known as “that Toronto mayor who smoked crack on video while in office”). Doug, who has been investigated by the Globe and Mail for his own alleged past as a teenage hash dealer, campaigned for office in part on his opposition to SCS, along with austerity and privatization policies.
Doug Ford’s Conservative government has enacted swift, brutal policy and funding changes broadly in line—in their emphasis on stripping protections from the most vulnerable—with Thatcherism or the US Republican Party.
So what happens when you take a state in which an accelerating overdose crisis has been somewhat mitigated by a range of harm reduction policies and a fairly strong social safety net—and then you dramatically worsen social determinants of health such as poverty, and access to healthcare and housing, heralding a more typically American, law enforcement-centered approach to substance use? And simultaneously cut back on those emergency harm reduction measures?
I visited the OPS (Overdose Prevention Site, a bare-bones, provincially funded version of an SCS) at St. Stephen’s Community House in downtown Toronto the week that it opened last May. One year later, I return after the provincial government abruptly pulled its funding—along with that of five of Ontario’s other 21 existing sites, also ending the provincial legal exemption allowing them to operate.
All the sites scrambled to seek new legal exemptions from the federal government and to cobble together temporary funding: combinations of GoFundMe, shifting scarce host organization budgets, and neighborhood donors. As a result, an emergency public health response has been privatized. St. Stephen’s is funded until December; a legal exemption from the federal government will also take it through to 2020, says Tyler Watts, its coordinator of Overdose Prevention Services.
The local community in the fast-gentrifying Kensington Market neighbourhood was welcoming even from the start, largely appreciating that the facility prevents many community harms. “The businesses here aren’t equipped to deal with overdoses in their washrooms, which was happening before we opened,” says Watts. He has seen barely any public illicit drug use in the area since the site opened last year.
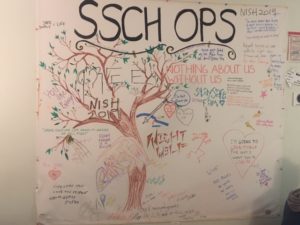
We’re sitting in the chill-out room next to the OPS. The room itself has two seats where people can sit to inject; clean syringes; naloxone; mirrors. The chill-out room is decorated with a mural inscribed with messages from clients; a photo of Crystal Papineau, a homeless woman who died in a preventable accident on a brutally cold night this winter.
There is also a large photo of Angela Kokinos; that wasn’t there last year, either. The last time I was here, I spoke with Kokinos, a vibrant, newly-abstinent 41-year-old. She died of an overdose in September—at home, not at the OPS. Watts tells me now, “When Ang died, I didn’t think we could withstand it any more.”

The small, tight team of overdose prevention workers considered closing the OPS for a day or two to mourn. Ultimately they decided they could not risk lives by not being there when people showed up first thing in the morning.
In Toronto, overdose deaths in these first few months of 2019 have nearly doubled.
The drug user population, which overlaps substantially with the local frontline overdose prevention worker population, was already suffering severe burnout when Doug Ford was elected in June of last year.
“People are exhausted,” says Franky, an injection drug user who also staffs an OPS in Ontario (she isn’t allowed to speak on behalf of her employer, so Filter agreed withhold its name as well as her last name). “There’s just been an intense amount of stress and anxiety and grief.”
And then there’s the impact in the north of the province. Mae Katt, nurse practitioner at Dennis Franklin Cromarty, a high school for First Nations students in Thunder Bay, Ontario, explains that she sees young people who often come to Thunder Bay from much smaller communities in the far north, unprepared for life in the city. Specifically, the city has astonishingly high rates of racism and violence against First Nations people, a dearth of safe, affordable recreation options, and a lot of illicit fentanyl in the drug supply.
The government has now cut a range of programs that would provide some protection to Katt’s patients. It has also made some medication-based treatment for addiction more expensive for low-income patients, Katt says—removing brand-name Suboxone from the Ontario drug benefits formulary and forcing healthcare practitioners to prescribe higher doses of the generic version to their lower-income patients, who must pay an extra 25 percent that was previously covered by the drug company.
Perhaps worst of all, the climate is increasingly hostile to First Nations people and people who use drugs. “I find the hate right now is really detrimental to every person in Ontario,” Katt says. For her patients, that’s an extra burden they don’t need. “They’re in a world where they feel the shame of having to be a drug user. Even if they’re in treatment they feel this stigma.”
Past Cuts Sowed the Seeds of Today’s Disaster
Back in 1995, Ontario’s newly-elected provincial Conservative Party set about restructuring the province with changes they called the “Common Sense Revolution.” Premier Mike Harris made devastating cuts to Ontario’s previously-strong social safety net, while weakening worker health and safety protections. Readily available opioid painkillers were an alternative.
“Harris disenfranchised tens of thousands in this city alone,” says James, who asked that his last name not be used. He was using heroin and became homeless in Toronto as a result of the Harris cuts. “That led to widespread poverty, persistent unemployment, recidivism—and if you check the figures it was the point when our homeless issue exploded in scope. Those victims are the homeless opioid users of this [current] crisis.”
“We made a permanent underclass, which Ford is basically targeting for extermination.”
Now in safe housing and taking Suboxone, James fears the new wave of drastic cuts will destabilize people like him who’ve just barely regained stability after years of extreme poverty. “We made a permanent underclass, which Ford is basically targeting for extermination.”
Dr. Ritika Goel, a Toronto physician who works with many patients who use drugs and who are insecurely housed, notes that the new cuts come against a background of services that never returned to pre-Harris levels.
“Income,” she notes, “is the number one determinant of health.”
Changes that will affect her patients’ health now include making it harder to qualify for disability benefits (which will reduce income for most OPS regulars), and cutting other income support programs; reducing incentives for developers to build affordable housing; loosening regulations protecting tenants from eviction; cuts to funding for subsidized childcare in Toronto; a dramatic but still-opaque restructuring of the provincial healthcare system; cuts to legal aid; and erosion of worker protections and worker safety oversight. Public health units are facing millions of dollars in cuts, and their numbers are to be slashed from 35 to 10.
Dr. Goel’s insecurely housed patients who use drugs already experience high rates of diabetes, high blood pressure, chronic obstructive pulmonary disease, smoking-related diseases, hepatitis C, HIV, liver disease, skin-related infections, endocarditis, PTSD, depression, anxiety, schizophrenia and bipolar disorder. And that’s before adding the overdose issue.
Overdose rates in Ontario, Dr. Goel explains, are already much higher than actual patterns of drug use would predict—likely the result of illicit fentanyl and other contaminants in the drug supply. “People are being poisoned at this time.”
As in the US, where a generation of older heroin users are dying of fentanyl and polydrug overdoses, survivors of Ontario’s Common Sense Revolution are now succumbing—along with their younger peers. Less risky opioids became dramatically harder to acquire following the introduction of tamper-proof OxyContin to Canada in 2012, driving a move to riskier, more potent illicit substances.
A Bleak Near Future
Other jurisdictions provide hints of what might happen next.
In the UK, a pilot heroin-assisted treatment program ran between 1982 and 1985—with no overdose deaths among its 450 participants. When the program was cancelled, 41 patients died within two years, among other health harms.
In Portugal, decriminalization and a range of harm reduction measures slashed rates of HIV and hep. C and dramatically reduced injection drug use. But between 2010 and 2014, austerity measures resulted in cuts to the harm reduction part of the plan, as well as a general increase in misery among marginalized drug users. Injection drug use has climbed again to the point that the country has finally opened its first SCS, a measure previously considered unnecessary.
“People know they are under attack.”
In Ontario, “people are going to die should these cuts have their effect,” says Watts, echoing Toronto’s medical officer of health, Dr. Eileen de Villa, who has also predicted deaths if SCS are forced to close.
“When you shut down an established service, you put people at risk,” Dr. Goel agrees.
As each new cut or change comes into effect, we can expect to see the impact in infectious disease rates, public drug use, public misery, punitive law enforcement response and finally, preventable deaths.
Dr. Goel describes a climate of fear among her patients. “People know they are under attack. They know cuts are happening and they know it’s going to affect them.” She doesn’t want to speculate on the impact of this stress on drug use patterns or recovery, saying only that people turn to different coping mechanisms in the face of an anxiety that is “totally warranted.”
“People who use drugs know that the Ford government is not a friend to them.”
Jessica Hale is a member of the Ontario Coalition Against Poverty and a nurse practitioner at another Ontario OPS that can’t be named. She puts it like this: “The whole issue with the cuts is that the community was already in absolute crisis.”
The site where Hale works, which unlike St. Stephen’s faces constant, sometimes aggressive opposition from local property-owners and businesses, serves a large population of Indigenous people and women of color. Some 60 percent of clients are women who are precariously housed or homeless (Hale’s site collects formal data on gender and age only, so most of this is her personal observation). The site has hosted 2,000 injections that would otherwise have taken place in parks, bathrooms, stairwells and alleys, she says.
Overcrowded shelters and an increase in evictions as neighbourhoods gentrify and housing prices skyrocket have been accompanied by an increase in pressures from police, who push homeless drug users out of parks, streets and other public places. Increasingly, they are not allowed to be anywhere.
Defiance Against the Odds
Most people I spoke with described a climate of anxiety, fear and extreme stress among people who use drugs in Ontario, particularly those who are poor and insecurely housed or homeless. But they also describe a sense of defiance.
Mae Katt, working with teenagers in Thunder Bay, believes that “their determination to change their life is much stronger than cuts.” She describes one patient—a single dad on Suboxone, who had to cancel plans to advance his education due to the government’s closure of a groundbreaking basic income pilot—who, she says, is seeking other options to improve his family’s life.
Despite cuts to most of a CA$500 million mental health and addiction budget intended in part as a response to the opioid-involved overdose crisis. And despite a legacy of residential schools in Ontario that—through family separation, widespread abuse and attempted cultural genocide—weakened social protection against addiction (Canada’s last residential school closed in 1996), Katt declares, “I don’t want to give Ford that much power to say that he will cause my patients to relapse.”
“I think people are really fed up,” Dr. Goel says. “Communities of people who use drugs have experienced so much trauma in the last few months. People are reaching a tipping point.”
“We have to take care of each other. Lord knows nobody else is.”
As I write these words, harm reduction and drug user communities in Toronto are reeling from the overdose death of Leon “Pops” Alward, one of the original group of drug user activists who brought SCS to Ontario with an illegal, volunteer-run site opened under a tent in a Toronto park in summer 2017. Ultimately, that initiative forced governments to belatedly acknowledge the public health crisis here, and to publicly authorize and fund the emergency response services that are now being cut back.
“It’s a public health crisis that’s not being treated as a public health crisis, that’s being put back on community and agencies and individuals to manage,” says Watts. “I had big plans for case management, better wraparound services, talking groups, harm reduction training. Instead of fulfilling all of those pieces, we’re always worrying about where the next dollar is coming from.”
At a large demonstration against the cuts to OPS in Toronto in April, I watched people shed tears as they spoke of loved ones lost to overdose. Demonstrators hugged each other and spoke defiantly. Angela Kokinos’ face was on a sign held aloft (pictured top) as the crowd marched from Queen’s Park, the provincial legislature, to the office of Ontario’s Medical Officer of Health, where they staged a die-in.

“We have to take care of each other,” Watts says. “Lord knows nobody else is.”
All photographs by Carlyn Zwarenstein





Show Comments