Four gentrifying Boston neighborhoods—Roxbury, Dorchester, the South End and South Boston—collide and form the intersection of Massachusetts Ave and Melnea Cass Blvd, named for a revered Roxbury civil rights leader. For short, “Mass and Cass.”
The area is described pejoratively as “Methadone Mile” and non-pejoratively as “Recovery Road.” One thing is clear, Mass and Cass is ground zero for twin wars: the wars on people who use drugs and people experiencing homelessness.
Deafening traffic noise from MBTA buses, flatbed tractor-trailers, cars, ambulances and police vehicles with sirens on full blast provides the intersection’s jarring soundtrack. The timing of traffic lights is confusing. Sixteen lanes of traffic converge on one of Boston’s five most dangerous intersections for pedestrians and cyclists, with an average of at least two injuries per month. It is this hazardous crossing that hundreds of people who are unhoused, using drugs and experiencing severe mental health issues must traverse daily to access services.
On a sizzling, sticky day last summer, the stretch is crowded with people socializing and taking care of business. A man rides by on a blue Citi Bike with a syringe between his teeth. A woman is hugging someone who is crying; I overhear that a good friend just died of an overdose. People pass by with the assistance of wheelchairs, canes, rolling walkers, plastic boot casts and back braces.
Sellers offer “Johnnies, Addies, Klonopins, Dubs.” A woman in a stained, gray sweat suit rolls by in a broke-ass wheelchair. She’s smoking and selling K2. A man carrying a black backpack announces, “Newports.” “How much?” I ask. $10. Menthol cigarettes are banned in Massachusetts and a bustling illicit market has sprung up, supplied by neighboring states.
A mobile sharps team is picking up discarded syringes. A church group set up a rack of free clothing, where they’re also handing out fresh fruit and bottled water. People offer each other snacks, cigarettes and face masks.

Two Colliding Worlds
Two opposite worlds face off against one another here. On the Newmarket Industrial District side of the divide, there are two methadone clinics: Boston Comprehensive Treatment Center and Health Care Resource Centers Boston. They sit amid a polluted, deindustrialized no-man’s-land of empty parking lots, and abandoned warehouses behind barbed wire fences or motorized metal gates with slates in the shape of spears.
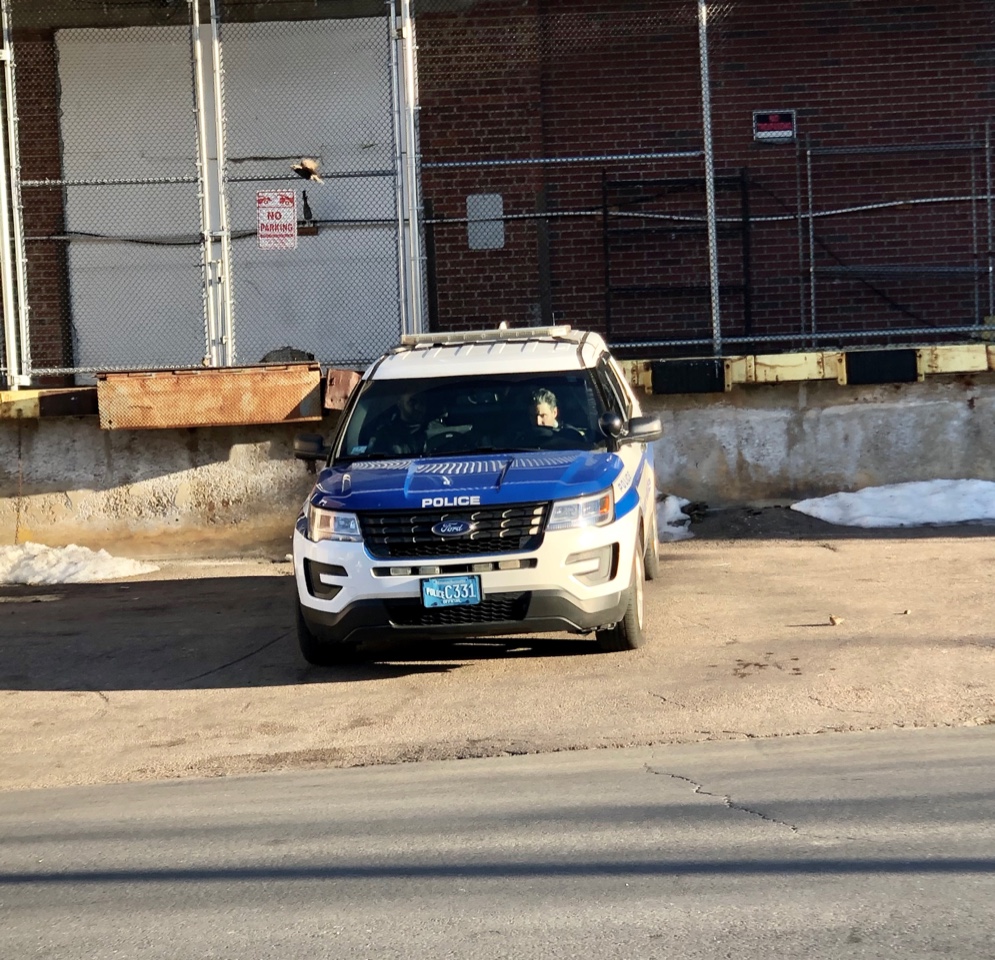
They’re joined by a City Wide gas station, Bubbles Car Wash, the storefront Universal Church and fast food outlets. Tractor trailers and rusted shopping carts full of disintegrating electronic junk dot the landscape. Piles of garbage, cigarette butts and syringes carpet the ground. No trash cans, let alone sharps containers. Side streets have only one narrow sidewalk and few street lights. No place to sit down. Signs warn no parking, no stopping, no smoking, no trespassing, no loitering and POLICE TAKE NOTICE. Another announces, “All activities monitored by video camera.”
The area is a hollowed-out, heavily policed, mini surveillance state, and a textbook example of hostile architecture. And this is where hundreds of people must rush six days a week to line up outside in the early-morning darkness to get methadone. It speaks volumes about the oppression of methadone patients that these clinics are found in such spaces.
The math, as always, favors punishment and prison.
Looming over them all is the enormous Suffolk County House of Corrections. It has 674 cells, 1,892 beds, serves thousands of hot meals daily and cost $115 million to build in 1990.
Down the street, the Southampton shelter for men has only 400 beds; the Woods-Mullen shelter for women has just 200. No hot food is served. The math, as always, favors punishment and prison.
It’s common for people to cycle through all three institutions here—prison, shelter, methadone clinic—over and over.
The other side of the Mass-and-Cass divide is anchored by the mighty Boston Medical Center (BMC). It consists of historic brick buildings with green-trimmed roofs; of brutalist concrete buildings mixed with gleaming modern ones with light-filled atriums; of glass pedestrian bridges and pavilions named for wealthy, white male philanthropists.
It’s Boston’s “safety-net” hospital, (code for people of color, people who are poor and uninsured) and home to the level-one Klarman Emergency and Trauma Center. All the medical specialities vital to human health are found in the blocks surrounding the hospital, with a wealth of resources devoted to addiction medicine. The Grayken Center for Addiction offers office-based Suboxone prescribing, inpatient detoxification and behavioral health services. There is even an urgent care program called Faster Paths to Treatment.
People with complex medical needs shuffle and stagger past inaccessible healers.
The Boston Medical District, with its heliport and its deep bench of trauma experts, is smack-dab in the middle of an open-air drug scene. Hundreds of unhoused people use drugs in the nooks and crannies, stairs and entrances of BMC buildings, the ambulance bays and loading docks.
On the sidewalks, medical personnel in scrubs with lanyards dangling from their necks walk by human beings nodding off, people clearly in mental distress or physical pain. One man in a wheelchair picks at open sores on his swollen, gray feet. Another walks in circles over and over, making animal noises. Ambulances with ear-splitting sirens race through the streets.
It’s a stunning contradiction that people with complex medical needs shuffle and stagger past inaccessible nurses, doctors, pharmacists, public health experts, social workers and psychologists, every single day. Healers stepping over suffering humanity. This is the danger: that the public and health care workers will lose empathy when year after year they see people violate social norms like injecting drugs in plain view, defecating or urinating on sidewalks and acting in troubled or aggressive ways.
Collapsing Services and COVID
The situation worsened in 2014 with the abrupt closing of a homeless shelter and the Andrew House Detoxification Center on Long Island, which was connected by bridge to the neighboring city of Quincy. The bridge was closed that year because it was near collapse; it’s estimated that over 700 people were dumped onto the streets.

To many, the problems seem intractable. But there is a solution. Boston is one of the richest cities in the country and has the resources to house everyone. Boston Mayor Martin J. Walsh has allocated millions to preserve and create affordable housing, but not enough: The number of unhoused people has not significantly decreased.
Around the city, the residential construction sites most in evidence are for luxury high-rises like Bullfinch Crossing. According to the website, “Bullfinch Crossing reconnects iconic downtown Boston neighborhoods and propels this heavily transit-served site forward into a 21st century global center.” Two glass towers with over 800 housing units will anchor the development. None of them will be affordable. On the South Boston waterfront another new neighborhood was created for the rich: the Seaport District. At the opulent St. Regis Residences, prices for a non-penthouse condominium with harbor views start at $2 million. Their tagline: “Live as you wish.”
COVID exposed massive inequality in the US in a way that was harder than ever to deny.
COVID-19 terminated the indoor ecosystem of services to people at Mass and Cass and forced the city to relocate them. “Because of the pandemic, we brought services outside in March,” Jennifer Tracey, the director of the Mayor’s Office of Recovery Services, told Filter. “The people we serve had to have access to bathrooms and hand washing. When a “comfort station” was created to meet this need, “the demand was so high we had to hire additional staff, including medical.”
But COVID did something else. It exposed massive inequality in the US in a way that was harder than ever to deny. On display for all to see was the enormous population of people who are homeless, hungry, uninsured, mentally ill, destitute and struggling with addiction. Moreover, the pandemic revealed the irrationality and cruelty of a means-tested welfare state that doesn’t help people in “normal” times, let alone now. Directives to seek medical attention if you are symptomatic for COVID-19, to shelter in place and practice social distancing are an insult to those who are uninsured, live on the street or sleep in crowded shelters.
The Comfort Station
Standing outside the comfort station, I asked Lisa,* a Black woman who was waiting there, what was going on inside. “This is a safe haven for drug users,” she explained. “A nurse watches you while you shoot up and makes sure you are safe.”
Lisa held her nose, crinkled up her face and cautioned me not to use the Porta-Johns. I ventured inside, to a small outdoor space with tents, jam-packed with people standing or sitting on the ground in various stages of shooting drugs. Parked on the left against a chainlink fence were racks full of sterile injection equipment. Three gray, portable sinks weren’t working, so instead, people were using a garden hose to wash. Several staff were on site, handing out supplies, answering questions and troubleshooting.
As well as serving as an unsanctioned, outdoor overdose prevention site, the comfort station functioned as a psychiatric drop-in center. Many people there displayed a range of what appeared to be psychotic symptoms, from mild to severe. People I spoke with seemed under-medicated, over-medicated or not medicated at all. As I stepped outside, a fight began between two men, and a woman intervened to break it up.
On the sidewalk I met Brian.* “It’s just another day on the avenue,” he said. “It’s a carnival.”
From his duffle-bag, he took out a large, amber prescription bottle, popped the top off and fished out a couple of capsules of gabapentin, the anti-seizure medication. They cost $1 per pill. “Gaba enhances the effects of other drugs,” Brian told me while making a quick sale.
“Why don’t the housing the homeless people come down here? This is where we all are.”
We moved around the corner to Albany street and found shade in front of the Maxwell Finland Building. Embossed above the entrance: Boston Public Health Commission. A small group of people were preparing to inject drugs, eating McDonald’s burgers, washing up (there were two portable sinks that worked), getting dressed and sleeping. It was like an outdoor apartment.

Brian, who is white, explained that he used heroin for over a decade in an attempt to “fix a feeling with another feeling.” Suboxone helped him stop, and he’s only returned to using one time, “My son helps me to not use.”
With a mix of resignation and frustration, Brian talked about being homeless for five years. Recently, he’d learned that an application for housing had been sent to the wrong address.
“Why don’t the housing the homeless people come down here?” he asked. “This is where we all are. Come here and help us apply for housing. Why do we have to go to an office?”
In yet another absurd contradiction, directly across from the Comfort Station is the Hampton Inn & Suites: 175 air-conditioned rooms, an indoor pool, free WiFi and complimentary breakfast. Why not house people there during a deadly pandemic?
Liberty and Law Enforcement
I returned to Boston in October. I know the city well, having lived there for a decade. The “Cradle of Liberty” has a rich political history. The siege of Boston opened the American Revolutionary War. In the famous Boston Tea Party, the Sons of Liberty dumped chests of black tea into the harbor because they believed there should be no taxation without representation. The city is steeped in the notions of freedom and personal liberty of which the ubiquitous American flag is a potent symbol.
But along Mass and Cass, these notions are illusive. The people I spoke with are not free. Their lives are destabilized by chronic homelessness, by episodic stints of incarceration, by social policies and drug laws that punish and leave them without basic life necessities. They are perpetually stuck on the bottom rung of Maslow’s Hierarchy of Need, struggling to meet the essential human requirements of housing, food, water and clothing.
He has untreated PTSD and an opioid use disorder, and isn’t wanted on Long Island or off.
Steve,* a Black man, had LOVE tattooed across his knuckles and several crosses on thick string wound around his neck. He wore Mickey Mouse pajama bottoms and a t-shirt emblazoned with the face of jazz trumpeter Miles Davis. We spoke through a chain-link fence on Mass Ave while he rearranged various items in plastic bags.
Steve reached inside a big bulge in his pants and pulled out a hat, scarf and gloves. He unleashed a bitter, angry and confusing monologue about his doomed attempts to secure housing, evictions, his own overdoses, and losing “lots of friends to overdose.” He has untreated PTSD and an opioid use disorder, and isn’t wanted on Long Island or off.
Leaving Steve, I walked to the comfort station—to find it gone! Not a trace of the community or the chaos remained. It had been erased.
That’s when I ran into Frosty Frost, a stylish, middle-aged white trans woman carrying a black and gray Prada handbag, milky-white hair combed back from her forehead. Frosty informed me that the comfort station had moved a few blocks away.
I immediately registered Frosty’s hard New England accent, with R’s dropped. When I broke out the quintessential catchphrase, “Park the car in Harvard Yard,” because I’m from Massachusetts, we two yankees broke into laughter.
Frosty was the unofficial “Mayor of Methadone Mile,” she said. A presence in the area for years, she demonstrated an encyclopedic knowledge of local drug markets and the history of the US War on Drugs. She offered to be my tour guide, and together we headed toward the relocated comfort station.

As we walked, the ubiquitous law enforcement presence made Frosty angry. She recalled a police raid in the area last summer called Operation Clean Sweep. It was an assault on the homeless community at Mass and Cass. Officers destroyed sleeping encampments and threw wheelchairs into garbage trucks. They detained people until they showed ID, then scanned them for outstanding warrants. Over 30 people were arrested. The Massachusetts ACLU filed a lawsuit against the city.
Not everyone opposes the police presence. “The police have a new street outreach team of seven, trained on crisis intervention, recovery coaching and they work really closely with us in the neighborhood,” Tracey said. “That team has been very helpful in the success of the comfort stations and works with us to get people into treatment.”
But why are the police, who harass and arrest people, doing street outreach? The movement to defund the police rightly identifies that as a major problem. When people with untreated mental health issues encounter law enforcement, they are 16 times more likely to be killed than the general population, and people of color are at even greater risk. Resources and responsibilities to assist vulnerable groups need to be shifted away from the police and given to peer advocates and professionals.
Engagement and NIMBY-ism
After carefully crossing Melnea Cass Blvd, Frosty and I took a left onto Atkinson, a quiet side street off of noisy Mass Avenue. City officials had assembled a space where people could use drugs, plus tented areas with picnic tables, a shower trailer and hand washing stations with soap dispensers and paper towels. A gigantic white tent in the back contained the engagement center. Staff wore red “Engagement” T-shirts with a black arrow pointing up. Loud conversations and hip-hop music filled the air.
As Frosty and I talked, she was continually interrupted by people saying hello, asking to use her cell phone and whether she knew who had drugs for sale. Frosty used to sell drugs, and told me with a sly smile that her business was called, “Frosty’s Fine Pharmaceuticals.”
“People are tired of being moved along all day. So we built a space that would be like a living room.”
When she left me for a few minutes to help a friend, I headed to the engagement center, sat down at a table and took in the action in the cavernous space. It was heated by cylindrical aluminum duct pipes along the ceiling that made loud, soothing white noise. The center contained necessities for those who don’t have a home: charging stations, chairs, microwaves, two flat panel TVs, computers, bathrooms, showers, coffee, Café Delight Non-Dairy Creamer packets, sugar, styrofoam cups, snacks and water dispensers. People were mopping the floor and sweeping up trash. A few were sleeping off in the corners. The vibe was chill.

“People don’t have a place to be during the day,” Devin Larkin, a social worker and the bureau director for Recovery Services at the Boston Public Health Commission, told Filter. “They’re on the street and they use sidewalks to do what we do in our living room. They are tired of being moved along all day. So we built a space that would be like a living room.”
The center is also designed to eliminate bureaucratic barriers to health care and drug treatment. Wound care, COVID-19 and HIV/STI testing, PrEP initiation, same-day detox, buprenorphine induction and sedation monitoring are all available. Staff I talked with off the record pride themselves on the fact that no one has ever overdosed and died on their watch.
It’s easy to see the principles of harm reduction in action at the engagement center. There are no security staff policing the space, people sleeping are left alone, and people can refuse medical or psychiatric services. “We are meeting people where they’re at and providing services that are acceptable to them,” said Larkin. “We ask, ‘What do you need today?’ whether it’s clean socks or a medical visit.”
The next day I got on a rusty old Orange Line train and exited at the Massachusetts Avenue stop. I walked five blocks past beautiful, gut-renovated brownstones with languid staircases and massive, wooden double doors. Signs on several buildings advertised, BRAND NEW LUXURY APARTMENTS FOR RENT.
Many of the people who occupy these sumptuous homes want the unhoused people living a few blocks down in shelters at Mass and Cass to get out. The South End-Roxbury Community Partnership has held a series of weekly protests with mixed messages. Placards proclaimed, “Mass Cass is a Public Health Crisis” and “Recovery is Possible”—but also, “Make the Community Comfortable for All!!!,” “No More Poop on our Stoop. Enough!” and “No More Needles.”
The group wants the Long Island Bridge rebuilt so drug treatment and shelter services can be restored out there. It’s classic NIMBY-ism. But not to be outdone, the mayor of Quincy is opposed to services being reopened on his turf.
The South End-Roxbury Partnership’s acknowledgment of a public health crisis is performative, earning them positive PR while putting pressure on city officials and the police to crack down. The endgame for such NIMBY groups is to oppose the creation of new services and close or relocate existing shelters and drug treatment programs, especially methadone clinics.
“If you’re homeless and you’re creating any kind of discomfort for other people just by existing,” said Dr. Joe Wright, director of addiction treatment at Boston Health Care for the Homeless, “the likelihood is that you will be pushed in one way or another down to the zone where the city has decided that they’re gonna push folks.”
That zone is “Methadone Mile.” The problem is the lack of permanent, affordable housing and everyone knows this. “You can go to drug treatment and do better,” Larkin said, “but if you are still living in a shelter, the quality of your life is hard.”
And imagine how hard it must be for people with a substance use disorder to stay in a shelter in an area where cheap drugs are on sale 24/7.
“The wait list for housing is long,” she added. “We are working closely with housing agencies to promote harm reduction and drug-user health to ensure that the people we work with have access to housing.”
Mass and Cass is an infuriating example of how the preventable is not prevented.
So hurry up and build public housing, Boston! And if the neighbors don’t like hundreds of people lining up to get a dose of methadone six days a week, close the clinics and create a pharmacy-based pick-up system that doesn’t silo and stigmatize methadone patients. If the gentrifiers don’t like to see people injecting drugs or syringes on the ground, demand safe consumption sites that offer people dignity and prevent them from dying. If owners of luxury brownstones don’t want shit on their stairs, install free public restrooms like the Portland Loo, a stand-alone, secure bathroom.
Mass and Cass is a community united by trauma, tragedy, tenderness and toughness. It is where homelessness, chronic mental health problems and the overdose crisis combine in degrading and deadly ways. It is an infuriating example of how the preventable is not prevented.
Frosty was waiting for me at the comfort station. We stood across from a bright blue sign that listed Community Agreements:
*Please use the restroom for its intended purpose.
*Use language that is considerate of others. This space should be safe for everyone.
*Please keep weapons or objects that could harm others out of the space.
*Do not share medications.
*Selling or purchasing items (clothes, cigarettes food, etc.) is not allowed in the space.
She wasn’t sure that anyone actually read the agreements. At least two were not being honored. I saw people sharing prescription medications and selling soda, socks and cigarettes. It shouldn’t be surprising; participation in the illicit economy is central to the survival of people who are locked out of the licit economy.
“Washing your hands isn’t going to work when you are sitting outside on the ground.”
Frosty and I walked over to the fenced area where dozens of people were in various stages of injecting, and had a discussion about dignity and drug use.
According to Frosty, dignified drug use was “not only privacy, it’s a safe, clean environment to use in. They give us clean supplies but they don’t give us a clean environment to use them in. Washing your hands isn’t going to work when you are sitting outside on the ground in the dirt, mud or the rain. You might be around vomit, shit, piss, blood. We need a place indoors with medical personnel that is sanitized. That would be a helluva lot better than what we have now.”
In the background a man was in a rage, pacing, shouting and swearing. It appeared that he had lost something. Frosty and I moved away but he kept moving toward us.
Then I realized it was Steve. I went over to talk to him. There was panic in his eyes. He said in a low voice, “I remember you. How come you walked away from me yesterday?” I started to explain, but Steve walked off, continuing to pace and escalate.
It was 4:30 and the outside areas of the comfort station were closing for the day. Staff asked everyone to move to the exit. People scrambled to gather their bags, bedding and bikes. Police sirens started to wail.
Frosty said this was how it always ended; people were driven like cattle out of the area by the police.
A crowd was now out on Atkinson street. I saw a man rolling around on the sidewalk and then I heard Steve’s voice. He was standing in the street wrapped in a blanket, still raging.
A police car moved near the crowd with lights flashing and a voice over the PA system warned everyone to leave. People began to scatter in different directions. Frosty and I said our goodbyes. I watched as she drifted away down the street, her hair blowing in the cold autumn wind, and I couldn’t help thinking about that tagline: Live as you wish.

*Names have been changed to protect sources’ privacy.
Correction: This article was originally published on February 9, but temporarily removed the next day in response to community members’ concerns. A process including an independent reviewer then took place before republication on February 18. A paragraph in the original article, now removed and retracted, implied criticism—based on inaccurate information—of Boston Users Union (BADUU), which in fact no longer operates, and other local activism. Filter apologizes for the offense and hurt this misrepresentation caused. We are committed to acknowledging and correcting factual inaccuracies and unfair representations. We are working to improve our processes and policies in this area.
All photographs by Helen Redmond.





Show Comments